Role of Calcium, Phosphorus and Intact Parathyroid Hormone in Different Stages of Chronic Kidney Disease
Dilip Kumar Sah1, S S Haque2*, Sweta Shah3 and Shyam Sundar Yadav4
1Department of Nephrology, Birat Medical College Teaching Hospital, Tankisinuwari, Nepal
2Department of Biochemistry, Indira Gandhi Institute of Medical Sciences, Patna, India
3Department of Obesity & Gynecology, Birat Medical College Teaching Hospital, Tankisinuwari, Nepal
4Department of Internal medicine, Birat Medical College Teaching Hospital, Tankisinuwari, Nepal
- *Corresponding Author:
- S S Haque
Department of Biochemistry,
Indira Gandhi Institute of Medical Sciences, Patna,
India,
E-mail: sshaq2002@yahoo.co.in
Received date: March 03, 2023, Manuscript No. IPJCEN-23-16007; Editor assigned date: March 06, 2023, PreQC No. IPJCEN-23-16007 (PQ); Reviewed date: March 17, 2023, QC No. IPJCEN-23-16007; Revised date: March 27, 2023, Manuscript No. IPJCEN-23-16007 (R); Published date: April 03, 2023, DOI: 10.36648/2472-5056.8.2.185.
Citation: Sah DK, Haque SS, Shah S, Yadav SS (2023) Role of Calcium, Phosphorus and Intact Parathyroid Hormone in Different Stages of Chronic Kidney Disease. J Clin Exp Nephrol Vol.8 No.2: 185.
Abstract
Background: Chronic Kidney Disease (CKD) normally hampered homeostasis of serum phosphorus calcium and intact Parathyroid Hormone (iPTH). Secondary Hyperparathyroidism (SHPT) arises in most patients during the progression of CKD, which is characterized by increased blood PTH levels. The aim of the study was to evaluate the role of calcium, phosphorus and iPTH levels in various stages of CKD.
Methods: Using a cross-sectional study design, we evaluated serum biochemical parameters and haemoglobin concentration among 70 CKD patients and 50 healthy persons as controls attending our outpatient nephrology clinic. CKD was defined as a glomerular filtration rate less than 60 ml/min/1.73 m2 for 3 months or more, while anemia was defined as a Hemoglobin concentration (Hb) less than 11 g/dl.
Results: The mean age of the study participants was 52.5 ± 13.2 years and 40 (57.1%) of the patients were males. The most common causes of CKD were diabetic nephropathy (70%) and hypertension (30%). The mean serum calcium and mean iPTH were 8.01 ± 1.96 mg/dl and 139.92 ± 93.42 pg/ml respectively.
Conclusions: In our study statistically significant increase in the serum levels of intact parathyroid hormone, urea, creatinine, calcium and phosphorus in patients with CKD as compared with controls.
Keywords
Parathyroid Hormone (PTH); CKD; Secondary Hyperparathyroidism (SHPT)
Introduction
Calcium and phosphorous homeostasis requires integration of many organs within the human body such as parathyroid glands, kidneys and intestine. Parathyroid Hormone (PTH) produced by the parathyroid gland and it is composed of 84 amino acids with very short half-life (2 min-4 min), encoded by a gene on the short arm of chromosome 11 and its main role is to increase serum Ca level and it is measured using the second generation intact PTH assay which has the ability to detect various PTH fragments including full-length 1-84 PTH and large C-terminal PTH fragments, mainly 7-84 PTH, a fragment with hypocalcemic hormone actions, although the roles of each fragment on various systems in the body are not yet clear [1].
CKD intact Parathyroid Hormone (iPTH) progressively increases gradually leads to the imbalance of calcium and phosphorous homeostasis [2]. At early stages of CKD with increases in Parathyroid Hormone (PTH) that begin at estimated Glomerular Filtration Rate (eGFR) levels of approximately 45 mL/min/1.73 m2 and the plasma. PTH concentration is negatively correlated with Glomerular Filtration Rate (GFR) in patients with CKD. Around 80% of patients with GFR of less than 20 mL/min/1.73 m2 have an increased level of PTH [3]. In advanced stage Chronic Kidney Disease (CKD), progressive loss of nephrons impairs the vitamin D activation which inally causes calcium deficiency.
Secondary Hyperparathyroidism (SHPT) is a common complication during the progression of CKD, which alters the mineral and bone metabolism and also increases iPTH levels [4]. The criteria for diagnosis of secondary hyperparathyroidism are low-normal serum calcium, high serum phosphorous and elevated serum parathyroid hormone levels. It is associated with increased comorbidity including Renal Osteodystrophy (ROD), extra skeletal calci ication and Cardiovascular Disease (CVD), resulting mortality and adversely affects the quality of life of patients with CKD [5]. In stage 3 of CKD 40% incidence of SHPT is reported, 70% in stage 4 and >80% in stage 5 [6,7]. The iPTH maintain the homeostasis between calcium and phosphorus in the body. Therefore, routine evaluation of serum levels of calcium, phosphorus, iPTH and alkaline phosphatase play an important role in different stages of CKD especially 3-5. The aim of the study is to determine the role of calcium, phosphorus and intact Parathyroid Hormone (iPTH) in different stages of chronic kidney disease.
Patients and Methods
A total of 120 consecutively presenting pre-dialysis CKD patients attending renal outpatient were screened and 70 adults above 17 years age, of either sex, diagnosed with CKD (predialysis) were randomly selected as cases and 50 healthy persons as controls. Patients providing informed consent and patients with documented chronic kidney disease were included in the study. The study was carried out between October 2021 and May 2022. All participating patients gave written informed consent. About 10 ml of blood was obtained from each patient for the determination of hemoglobin concentration, serum protein, albumin, creatinine, urea, calcium, phosphorus, alkaline phosphatase and iPTH were routinely measured in the clinical laboratories using fully automated analyzer. CKD was defined as the presence of markers of kidney damage and/or eGFR of <60 mL/min/1.73 m2 for at least three months [8].
Statistical analysis
Comparison between means was carried out using the student’s t-test while comparison between percentages was carried out using chi square test. One-way Analysis of Variance (ANOVA) and Kruskal-Wallis tests were used to compare participants’ parameters across the stages of CKD. The level of statistical significance was set at a P value less than 0.05.
Results
A total of 70 patients and 50 as a control were included in this study. The mean age of the study participants was 52.5 ± 13.2 years. In our study, 40 (57.1%) were men and 30 (42.8%) were women. 35 patients (50%) were in the age group 40-60 years. Demographic characteristics are summarized in Table 1. Hypertension (70%) was the most common chronic morbidity among the participants followed by diabetes mellitus (30%).
| Sr.No | Characteristics | N (%) |
|---|---|---|
| 1 | Age in years | |
| 20-40 | 10 (14.28) | |
| 40-60 | 35 (50) | |
| More than 60 | 25 (35.71) | |
| 2 | Sex | |
| Male | 40 (57.1) | |
| Female | 30 (42.8) | |
| 3 | Etiology | |
| Hypertension | 49 (70) | |
| Diabetes mellitus | 21 (30) | |
| 4 | Stages of CKD | |
| Stages I&II | 8 (11.42) | |
| Stages IIIa | 13 (18.57) | |
| Stages IIIb | 14 (20) | |
| Stages IV | 14 (20) | |
| Stages V | 21 (30) | |
Table 1: Demographic details of the study participants (N=70).
The mean serum urea level was 78.98 ± 68.63 mg/dl when compare to control (22.01 ± 6.92), which was statistically significant (***P<0.0001). The significantly increased creatinine and urea levels were in conformity with the results obtained by Dirican, et al. who also observed that these values were increased when compared to controls [9]. The mean serum calcium level was 8.01 ± 1.96 significantly lower than control 9.1 ± 0.92 mg/dl, P=0.004 (Table 2).
| Parameter | Cases (n=70) Mean ± SD | Control (n=50) Mean ± SD | Standard error | 95% CI | P-value | t-statistic |
|---|---|---|---|---|---|---|
| Blood urea (mg/dl) | 78.98 ± 68.63 | 22.01 ± 6.92 | 9.753 | -76.2826 to -37.6574 | ***P<0.0001 | -5.842 |
| Serum creatinine (mg/dl) | 6.31 ± 4.98 | 0.86 ± .30 | 0.706 | -6.8481 to -4.0519 | ***P<0.0001 | -7.719 |
| Serum calcium (mg/dl) | 8.01 ± 1.96 | 9.1 ± 0.92 | 0.298 | 0.4990 to 1.6810 | **P=0.0004 | 3.652 |
| Serum phosphorous (mg/dl) | 4.93 ± 1.82 | 3.52 ± 0.71 | 0.271 | -1.9472 to -0.8728 | ***P<0.0001 | -5.198 |
| Serum protein (g/dl) | 6.92 ± 0.91 | 6.82 ± 0.73 | 0.197 | -0.4935 to 0.2935 | P=0.613 | -0.507 |
| Serum albumin(g/dl) | 3.6 ± 0.70 | 3.56 ± 0.54 | 0.149 | -0.3382 to 0.2582 | P=0.789 | -0.268 |
| iPTH (pg/ml) | 139.92 ± 93.42 | 51.02 ± 15.93 | 13.63 | -115.3632 to -62.4368 | ***P<0.0001 | -6.652 |
| Serum alkaline phosphatase (IU/L) | 98.13 ± 47.12 | 83.11 ± 29.68 | 7.553 | -29.9779 to -0.0621 | P=0.0491 | -1.988 |
| Note: Statistically significant as *P<0.05, **P<0.01 and statistically highly significant as***P<0.0001 | ||||||
Table 2: Biochemical parameters.
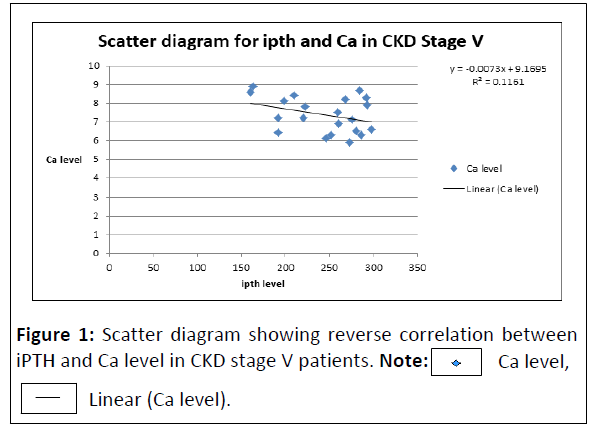
A reverse correlation was found between intact PTH and Ca level (r=-0.340), which indicates that the variables iPTH and Ca level are inversely proportional to each other (Figure 1).
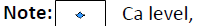
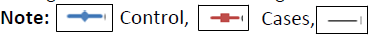
In our study, the increased levels of mean serum iPTH were present even in CKD stage I and II and it was related to low mean serum calcium level and progressive rise of serum inorganic phosphate from early to advanced CKD (Figure 2). Nasri, et al. have reported that there is a positive correlation of serum phosphate, Ca × P product and iPTH with serum calcium implying that there is a central role for phosphorus in calcium-phosphorus deposition in soft tissues like cornea and conjunctiva, underscoring further attention to phosphorus control in CKD patients undergoing hemodialysis (Figures 3 and 4) [10].
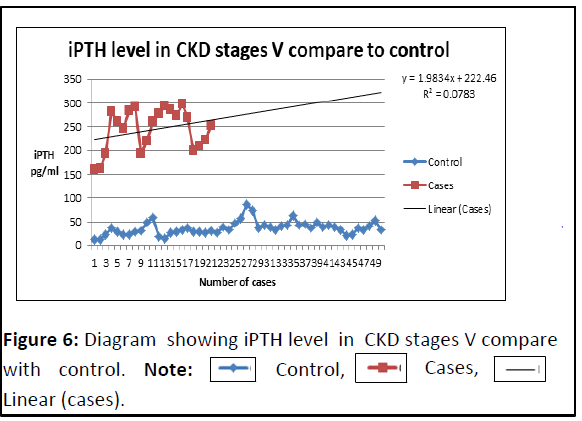
The level of serum iPTH was higher in CKD stage IV and V thus confirming the relationship between severity of hyperparathyro - idism and the degree of renal impairment (Figures 5 and 6) [11].
Discussion
Majority of the patients presented in late stages of CKD, with over 35% in stage IV and V. In relation to the co-morbidities, hypertension was 70% which was similar to the study by Abraham, et al. [12]. In our study the patients stage V of CKD (dialysis) had significantly higher chance of having secondary hyperparathyroidism when compared to nondialysis patients (stage I-IV CKD) similar studies conducted by Levin, et al. where patients belonging to stage IV and V had higher prevalence of secondary hyperparathyroidism when compared to the Stage I-III [6,13]. Malawadi, et al. in 2014 found that the serum iPTH (331.68 ± 204.99 pg/mL) was significantly higher in more advanced renal failure (CRF stage V), which confirms the relationship between severity of hyperparathyroidism and the degree of renal impairment, which was almost similar to our study [14].
In CKD stage V (dialysis) patients are most likely to have secondary hyperparathyroidism which was similar to our study [15]. As stages of CKD advances the level of intact PTH also increases, de Boer, et al. also observed increased iPTH levels as the stage of CKD advances [16]. The increased levels of mean serum iPTH may be related to reduction in serum calcium level and progressive rise of serum inorganic phosphate from early to advanced stages of CKD.
Conclusion
Parathyroid hormone serum level is high in CKD patients, more than one-fifth of the CKD patients had secondary hyperparathyroidism and significant association between stages of CKD and secondary hyperparathyroidism especially in patients belonging to stage IV and V and it is associated with mortality and morbidity in CKD patients and excessive suppression of parathyroid hormone with calcium-containing compounds and vitamin D leads to bone diseases. It is concluded that the estimation of serum iPTH and calcium and phosphorous helps for the diagnosis of secondary hyperparathyroidism in the early stage of CKD and to manage the future complications of chronic renal failure.
References
- Huimin C, Ying C, Changying X, Xiaoming Z, Yan Z, et al. (2018) Effects of parathyroidectomy on plasma iPTH and (1-84) PTH levels in patients with stage 5 chronic kidney disease. Horm Metab Res 50: 761-767.
[Crossref], [Google Scholar], [Indexed]
- Ritter CS, Slatopolsky E (2016) Phosphate toxicity in CKD: The killer among us. Clin J Am Soc Nephrol 11: 1088-100.
[Crossref], [Google Scholar], [Indexed]
- van der Plas WY, Noltes ME, van Ginhoven TM, Kruijff S (2020) Secondary and tertiary hyperparathyroidism: A narrative review. Scand J Surg 109: 271-278.
[Crossref], [Google Scholar], [Indexed]
- Cunningham J, Locatelli F, Rodriguez M (2011) Secondary hyperparathyroidism: Pathogenesis, disease progression and therapeutic options. Clin J Am Soc Nephrol 6: 913-921.
[Crossref], [Google Scholar], [Indexed]
- Melamed ML, Eustace JA, Plantinga L, Jaar BG, Fink NE, et al. (2006) Changes in serum calcium, phosphate and PTH and the risk of death in incident dialysis patients: A longitudinal study. Kidney Int 70: 351-357.
[Crossref], [Google Scholar], [Indexed]
- Levin A, Bakris GL, Molitch M, Smulders M, Tian J, et al. (2007) Prevalence of abnormal serum vitamin D, PTH, calcium and phosphorus in patients with chronic kidney disease: Results of the study to evaluate early kidney disease. Kidney Int 71: 31-38.
[Crossref], [Google Scholar], [Indexed]
- Andress DL, Coyne DW, Kalantar KZ, Molitch ME, Zangeneh F, et al. (2008) Management of secondary hyperparathyroidism in stages 3 and 4 chronic kidney disease. Endocr Pract 14: 18-27.
[Crossref], [Google Scholar], [Indexed]
- Abefe SA, Abiola AF, Olubunmi AA, Adewale A (2009) Utility of predicted creatinine clearance using MDRD formula compared with other predictive formulas in Nigerian patients. Saudi J Kidney Dis Transpl 20: 86-90.
[Google Scholar], [Indexed]
- Dirican M, Akca R, Sarandol E, Dilek K (2004) Serum paraoxonase activity in uremic predialysis and hemodialysis patients. J Nephrol 17: 813-818.
[Google Scholar], [Indexed]
- Nasri H, Baradaran A, Doroudgar F, Ganji F (2003) Relationship of conjunctival and corneal calcification with secondary hyperparathyroidism in hemodialysis patients. Iran J Med Sci 28: 86-89.
- Karl S, Jacob G, Barry MB (2013) Chronic renal failure. In: Kasper, Braunwald, Fauci, Hauser, Longo, Jameson, editors, Harrison’s Principles of Internal Medicine.
- Abraham G, Arun KN, Gopalakrishnan N, Renuka S, Pahari DK, et al. (2017) Management of hypertension in chronic kidney disease: Consensus statement by an expert panel of Indian nephrologists. J Assoc Physicians India 65: 6-22.
[Google Scholar], [Indexed]
- https://www.era-online.org/about-us/working-groups/ckd-mbd-working-group/
- MalwadiI BN, Suma MN, Prashant V, Akila P, Anjalidevi BS, et al. (2014) Secondary hyperparathyroidism in all the stages of chronic kidney disease in Southern Indian population. Int J Pharm Pharm Sci 6: 1-4.
- https://www.kidney.org/sites/default/files/02-10-4899_GB_SHPT-PTH_v8.pdf
- De Boer IH, Gorodetskaya I, Young B, Hsu CY, Chertow GM (2002) The severity of secondary hyperparathyroidism in chronic renal insufficiency is GFR dependent, race dependent and associated with cardiovascular disease. J Am Soc 13: 2762-2769.
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences
 (control)
(control)
 Linear (cases).
Linear (cases).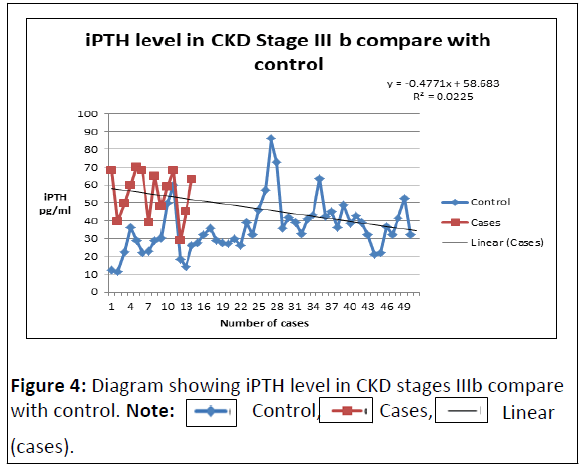
 (cases).
(cases).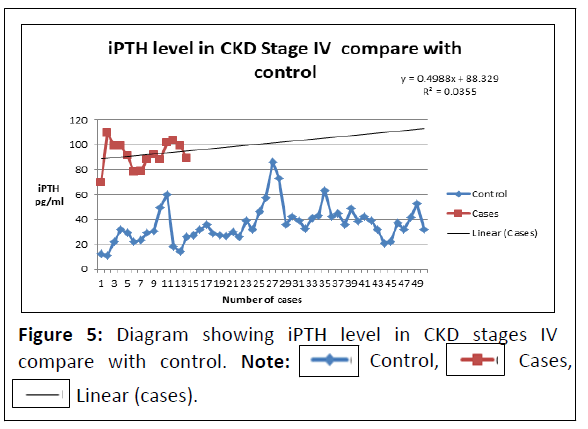
 Linear (cases).
Linear (cases).