Adrenocortical Oncocytoma: A Case Report and Review of Literature
Kato T1, Komiya A, Kamiya N, Ishikura H, Ichikawa T, Ito H
DOI10.21767/2472-5056.100016
Kato T1,2*, Komiya A1, Kamiya N1,3, Ishikura H3, Ichikawa T1 and Ito H1
1Department of Urology, Graduate School Of Medicine, Chiba University, Japan
2Department of Urology, Kuki General Hospital, Japan
3Department of Molecular Pathology, Graduate School of Medicine, Chiba University, Japan
- *Corresponding Author:
- Tomonori Kato
Department of Urology
Kuki General Hospital, 418-1 Kamihayami
Kuki, Saitama, 346-8530 Japan
Tel: +81-486-26-0033
E-mail: jpn3899kato@yahoo.co.jp
Received date: June 28, 2016; Accepted date: August 09, 2016; Published date: August 16, 2016
Citation: Kato T, Komiya A, Kamiya N, Ishikura H, Ichikawa T, et al. (2016) Adrenocortical Oncocytoma: A Case Report and Review of Literature. J Clin Exp Nephrol 1:16. DOI: 10.21767/2472-5056.100016
Copyright: © 2016 Kato T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
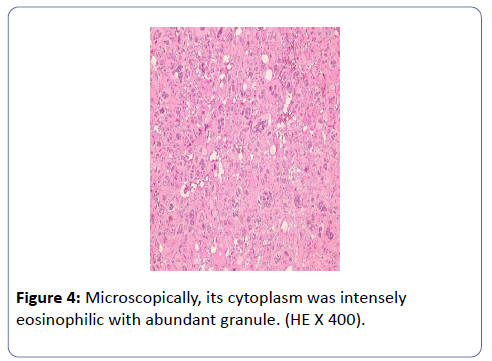
A 53-year old man was found to have a right incidental adrenal mass measuring 5 × 6cm. The patient underwent laparoscopic right adrenalectomy and the tumor was surgically removed. The histological diagnosis was oncocytoma, the cytoplasm of which was intensely eosinophilic with abundant granule. Oncocytoma of the adrenal gland is rare disease.Recently, the advancement of imaging techniques, especially the routine use of computed tomography (CT) and magnetic resonance imaging (MRI) lead to increased number of incidentally discovered adrenal masses including adrenocortical oncocytoma. In this report, the clinical features of adrenocortical oncocytomas are discussed.
Keywords
Adrenal cortex; Oncocytoma; Nonfunctioning adrenal tumor
Abbreviations
CT: Computed Tomography; MRI: Magnetic Resonance Imaging; Ad4BP: Adrenal 4 Binding Protein
Introduction
Oncocytoma is an epithelial neoplasm composed of oncocytic cells whose cytoplasm is packed with mitochondria [1]. This tumor is characterized by a histologic pattern of large eosinophilic cells with a granular cytoplasm. Oncocytomas may arise in various organs such as kidney, salivary gland, thyroid, adrenal cortex and parathyroid glands. Among them, oncocytoma of the adrenal gland is relatively rare [2,3]. In this manuscript, we report a case of adrenocortical oncocytoma and the clinical features of adrenocortical oncocytomas are discussed.
Case Report
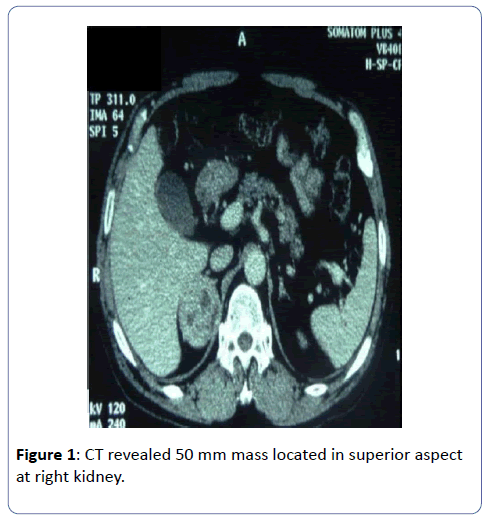
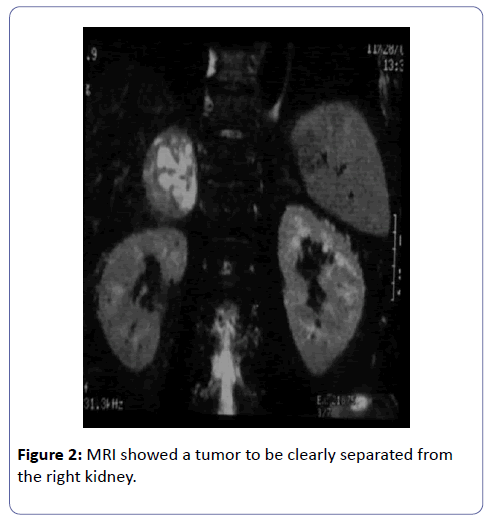
A 53-year old man was involved in a traffic accident and underwent computed tomography (CT). Incidentally, he was found to have a right adrenal mass measuring 5×6cm, which was enhanced irregularly and was located in superior aspect at right kidney (Figure 1). He admitted to our Hospital for evaluation of the mass. Magnetic resonance imaging (MRI) showed a tumor to be clearly separated from the right kidney. The mass showed hypointensity on T1-weighted imaging and isointensity to hypointensity on T2-weighted imaging (Figure 2). There was no evidence of metastatic disease on a chestabdomen CT scan and a bone scintigraphy.
The patient had a mild hypertension controlled with amlodipine. His blood pressure was 138/92 mmHg and pulse 66 beats per minutes. Physical examination was unremarkable. Routine laboratory studies were normal, including full blood count and urea and electrolytes. Hormonal data were also within normal limits, with the exception of slightly elevated serum noradrenalin at the level of 25 pg/ml.
Initially, pheochromocytoma was suspected due to hypertension and slightly elevated level of serum noradrenalin. However, the regitine test was negative and MIBG scan showed no abnormal uptake. In addition, to rule out functioning adrenal tumor, rapid ACTH test, captopril test and dexamethasone 1 mg suppression test were performed which were all negative. Preoperative diagnosis of right nonfunctioning adrenal tumor was made.
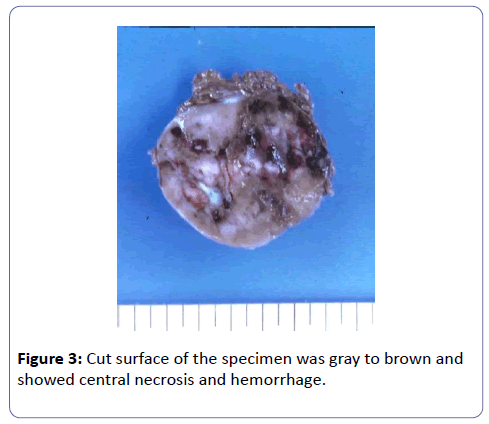
Subsequently, the patient underwent laparoscopic right adrenalectomy because its size exceeds 4 cm in diameter. The surgical specimen weighed 62 g. The tumor was surrounded by fibrous capsule which was successively attached to normal adrenal tissue. There was no extracapsuler or capsular invasion of the tumor. Cut surface was gray to brown in color and showed central necrosis and hemorrhage (Figure 3).
The tumor cells showed specific findings of the oncocytomas. The cytoplasm was intensely eosinophilic with abundant granule (Figure 4).
A few atypical cells with hyperchromatic nuclei were diffusely scattered, which suggests malignant potential. Mitotic rate of these atypical cells was greater than 5 per 50 high power fields. Occasionally, small areas of necrosis were observed.
The diagnosis of oncocytoma is further confirmed by immunohistochemical findings. The tumor cells showed a strong positive reaction for NSE and focal positive for chromogranin-A. Staining for cytekeratin(AE1/AE3), EMA, vimentin, and S-100 protein were negative.
To confirm adrenocortical origin, immunostaining for adrenal 4 binding protein (Ad4BP), a transcription factor of steroidgenesis, was performed [4]. The tumor cells were positive for Ad4BP, which indicated the tumor originated from adrenal cortex. On the basis of these observations, the final diagnosis was an adrenocortical oncocytoma.
The postoperative course was unremarkable. Considering high nuclear grade and atypical mitotic figures, we have continued postoperative follow up with imaging. However, the patient was alive and well without evidence of recurrence 10 years after surgery.
Discussion
Oncocytoma is an epithelial neoplasm composed of cells whose cytoplasm is packed with mitochondria [1]. Oncocytomas may arise in various organs, including the salivary glands, kidney, thyroid, parathyroid, and pituitary, however, oncocytoma of the adrenal gland have been rarely reported [5]. About 147 cases of adrenocortical oncocytomas have been reported in the literature [3,6].
Most of oncocytomas are nonfunctional and most are detected incidentally during imaging [3,6]. As the specific finding of oncocytomas, the presence of a central fibrous scar, leading to the ‘‘spoke wheel’’ pattern was seen on CT or MRI in about one-third of the patients [7]. However, the ‘‘spoke wheel’’ pattern cannot be used for differentiating adrenal cortical adenoma from adrenal carcinoma [8]. Therefore, the diagnosis is usually based on the pathological characteristics of the specimen obtained by surgery.
It is relatively easy to diagnose oncocytomas by lightmicroscopic examination for its unique histological characters. The histological characteristic of oncocytoma is the predominance of oncocytes in which the cytoplasm becomes eosinophilic due to accumulation of abnormal mitochondria [5].
Adrenal oncocytomas are usually non-functional and benign, and surgical removal is usually associated with an excellent prognosis. However, some cases has been reported to demonstrate clinically malignant behavior [3,9]. And some cases were suggested to have potentially malignant histological findings [10]. The Lin-Weiss-Bisceglia criteria have been developed for classifying adrenocortical oncocytic tumors histologically as benign, borderline malignant potential, and malignant [11]. According to these criteria, high mitotic rate, atypical mitoses, and venous invasion are defined as major criteria and larger sized tumor (>10 cm and/or >200 g), necrosis, capsular invasion, and sinusoidal invasion are defined as the minor criteria. If the tumor exhibits one or more of the major criteria, it is considered malignant. The presence of 1 to 4 minor criteria indicates uncertain malignant potential (borderline). If none of the aforementioned features are present, a tumor can be considered benign [11].
According to Lin-Weiss-Bisceglia criteria, our case has 2 major criteria positive (namely, nuclear grade and atypical mitosis). Considering high nuclear grade and atypical mitotic figures, we have continued postoperative follow up with imaging, and he had no evidence of disease for 10 years after surgery. Our case demonstrates clinically benign postoperative course.
Conclusion
The advancement of imaging techniques, especially the routine use of CT and MRI lead to increased number of incidentally discovered adrenal masses including adrenocortical oncocytoma. We believe that this case presentation could provide useful information on differential diagnosis of nonfunctioning adrenal tumors.
Acknowledgement
We thank Prof. Hironobu Sasano for An immunohistochemical evaluation of Ad4BP.
References
- Erlandson RA, Reuter VE (1991) Oncocytic adrenal cortical adenoma. Ultrastruct Pathol 15:539-547.
- Maximo V, Rios E, Sobrinho-Simoes M (2014) Oncocytic lesions of the thyroid, kidney, salivary glands, adrenal cortex, and parathyroid glands. Int J Surg Pathol 22:33-36.
- Mearini L, Del Sordo R, Costantini E, Nunzi E, Porena M (2013) Adrenal oncocytic neoplasm: a systematic review. Urol Int 91:125-133.
- Sasano H, Shizawa S, Suzuki T, Takayama K, Fukaya T, et al. (1995) Transcription factor adrenal 4 binding protein as a marker of adrenocortical malignancy. Hum Pathol 26:1154-1156.
- Chang A, Harawi SJ (1992) Oncocytes, oncocytosis, and oncocytic tumors. Pathol Annu 27:263–304.
- Wong DD, Spagnolo DV, Bisceglia M, Havlat M, McCallum D, et al. (2011) Oncocytic adrenocortical neoplasms-a clinicopathologic study of 13 new cases emphasizing the importance of their recognition. Hum Pathol 42:489-499.
- Tahar GT, Nejib KN, Sadok SS, Rachid LMM (2008) Adrenocortical oncocytoma: a case report and review of literature. J Pediatr Surg 43:E1-3.
- Tirkes T, Gokaslan T, McCrea J, Sandrasegaran K, Hollar MA, et al. (2011) Oncocytic neoplasms of the adrenal gland. AJR Am J Roentgenol 196:592-596.
- El-Naggar AK, Evans DB, Mackay B (1991) Oncocytic adrenal cortical carcinoma. Ultrastruct Pathol 15: 549-556.
- Botsios D, Blouhos K, Vasiliadis K, Asimaki A, Tsalis K, et al. (2007) Adrenocortical oncocytoma-a rare tumor of undefined malignant potential: report of a case. Surg Today 37: 612-617.
- Bisceglia M, Ludovico O, Di Mattia A, Ben-Dor D, Sandbank J, Pasquinelli G, Lau SK, Weiss LM. Adrenocortical oncocytic tumors: report of 10 cases and review of the literature. Int J Surg Pathol 2004; 12: 231-43.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences