Cost Effectiveness of a Community Based Innovative Model of Multi-Disciplinary Chronic Kidney Disease Care
Albert Kadri, Maher M El-Masri, Mohammed J Ibrahim, Colleen Bassett and Nicole Dziamarski
DOI10.21767/2472-5056.100059
Albert Kadri*, Maher M El-Masri, Mohammed J Ibrahim, Colleen Bassett and Nicole Dziamarski
Department of Nephrology, Vascular Health and Research Institute, Canada
- *Corresponding Author:
- Albert Kadri
Department of Nephrology, Vascular Health and Research Institute, Canada
Tel: 5197909088
E-mail: dr.kadri@careforkidneys.org
Received date: February 08, 2018; Accepted date: March 22, 2018; Published date: March 26, 2018
Citation: Kadri A, El-Masri MM, Ibrahim MJ, Bassett C, Dziamarski N (2018) Cost Effectiveness of a Community Based Innovative Model of Multi-Disciplinary Chronic Kidney Disease Care. J Clin Exp Nephrol Vol 3:8. DOI: 10.21767/2472-5056.100059
Copyright: © 2018 Kadri A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Patients with chronic kidney disease are at an increased risk of cardiovascular disease and the associated morbidity and mortality. This patient population is also associated with a substantial cost to the healthcare system with traditional hospital-based care management. The objective of this study is to investigate the cost effectiveness of providing community-based multidisciplinary clinic (MDC) care to this patient population. The goal was to evaluate whether the new model of care is associated with improved patient compliance with medical appointments, and can be delivered effectively within the community in a patient-centred fashion.
Design: In this retrospective analysis, participants in this study included patients started within the local regional program who needed dialysis chronically or until death and were followed for at least 3 months prior to dialysis. Comparison was made between those patients attending a hospital based clinic vs. a community based clinic with respect to optimal and suboptimal start rates, use of internet based educational resources was tracked, potassium, haemoglobin, calcium, phosphorus, PTH levels pre dialysis and patient attendance rates were measured as well.
Results: The results attained from performing this 15-month retrospective analysis showed that this community based model of care yielded similar results with respect to optimal vs. suboptimal start rates, laboratory parameters at initiation of dialysis, and may have been associated with increased rates of attendance to visits.
Conclusions: Our findings show that multidisciplinary care for advanced chronic kidney disease patients can be effectively delivered in a community-based model. This is likely to have significant cost benefits as well as increasing access to care for patients in rural communities or those who prefer to receive their care in a community setting.
Keywords
Kidney; Dialysis; Healthcare; Glomerular filtration rate
Introduction
Chronic kidney disease (CKD) patients are among the highest risk population for cardiovascular disease, and this continues to be the leading cause of death in this population. An estimated 3.6 million Canadians have, or at risk for CKD [1]. In 2009, there were nearly 38,000 Canadians on renal replacement therapy– more than triple the number in 1990, according to CIHR. It is estimated that 2.2 billion dollars are spent on dialysis in Canada annually. In our opinion, there is an escalating need as well as an opportunity for alternative models of community based care using available technology to decrease the health and financial burdens of managing CKD.
The overall objective of an alternative model of care for CKD patients is to better align the with the priorities of the Ontario Renal Network (ORN) with respect to patient-centred care in the community that is accessible, accountable, and cost-effective in achieving pre-defined quality indicators. The alternative community-based model of care focuses on pre-dialysis patients with the intent of enhancing accessibility and patient attendance with utilization of a novel community based approach to multi-disciplinary care combined with access to internet based educational resources for patients and families.
Guidelines for pre-dialysis care are based on the estimated Glomerular Filtration Rate (eGFR). According to guidelines between January 2015 and March 2016 patients were eligible for referral to pre-dialysis clinics when their eGFR was below 30. In 2016, the ORN redefined eligibility criteria for pre-dialysis funding. Eligibility for funding is currently given to patients where their 2-year risk of requiring dialysis is ≥ 5% or their estimated Glomerular Filtration Rate (eGFR) is <15 [2].
According to the ORN: “The goal of the pre-dialysis clinic visit is to provide management to: slow progressive GFR decline; prevent, monitor and treat the multisystem complications of CKD and co-morbid illnesses; and prepare for renal replacement therapy” [3]. This can be accomplished in community based programs that provide many added advantages to comparable hospital based programs. In addition to this goal, the ORN mandates patients are seen by three multidisciplinary health care professionals. A community based model can take advantage of existing community resources and strengthen ties within the community, especially between primary practitioners and front line auxiliary services (such as community pharmacies). Shifting outpatient care into the community is often much more cost-effective.
The challenges that currently exist with the growing population and escalating rates of CKD require innovative solutions to provide care that continues to be patient-centred and community based. There are many remote areas where people cannot travel to hospital-based multidisciplinary clinics. Components of care should be standardized according to evidence of effectiveness, yet often an individualized approach is necessary based on patient needs and preferences. In our opinion, the most important early intervention is education. This can be accomplished in many ways and we used a combination of on-site group and 1:1 education as well as the use of internet based resources to allow patients and family members to review information at their convenience as many times as needed.
A community based care model has vast potential for cost effectiveness compared to a standard hospital based model. There is also an opportunity to study whether improved access in a community setting can increase patient attendance and compliance. This is especially important in CKD which tends to be an asymptomatic condition until late in disease progression. Lack of attendance to clinic visits can lead to patients being lost to follow up and increased crash and suboptimal starts that in turn drive up healthcare costs. In addition there is also an opportunity to promote a ‘wellness culture’ in dealing with CKD rather than perpetuating an illness model which can be associated with outpatient hospital-based care programs which over time may enhance the uptake of independent dialysis modalities and reduce reliance on hospital based resources. Limited comprehensive community based pre-dialysis care models are available and fewer still have been studied to show their impact on patient indicators and outcomes [4].
This research was conducted in response to the recommendations of the Ontario Renal Network, and LHIN which endorsed this specific patient-centred model of care in the community with letters of support [5]. The goal was to evaluate whether the new model of care is cost-effective, associated with improved patient compliance with medical appointments, and can be delivered effectively within the community in a patient-centred fashion.
Methods
At the request of the LHIN and ORN [5], and Research Ethics Board (REB) approved retrospective analysis was conducted to compare data on the outcome indicators between patients with CKD who utilize hospital based models of care against those who are managed under an innovative community–based model of care. Only patients started within the local regional program who needed dialysis chronically or until deaths who were followed for at least 3 months prior to dialysis were included in the study. In this patient population the following outcome indicators were examined: (a) access to web based education, (b) attendance/no show rates and (c) optimal vs. suboptimal start rates on dialysis. Comparisons were made based on a 15- month study period to allow for an adequate sample size. Acuity scales, age, and other patient demographics were not used in order to ensure practice populations were equal. Descriptive statistics on each of the study outcome indicators were performed and compared to available statistics for a comparable hospital-based program. Below is a description of the two models of care:
Hospital based standard model of care
In this model of care, patients with an eGFR<30 are cared for in outpatient clinics in a hospital setting. This often can give the impression to patients who feel well and may be working full-time etc. that they are now too sick to be treated within the community. This in turn promotes a model of illness rather than wellness as patients tend to associated significant illness with the need to attend a hospital for care. Historically, attendance at hospital based clinics for CKD patients is less than optimal throughout the province. This leads to more patients ending up with suboptimal outcomes, more emergency room visits, more crash starts on to dialysis and less uptake of independent therapies. This is important given that currently in Ontario, given the amount of money spent annually on dialysis-related services.
When the kidney function of CKD patient declines significantly and there is anticipation that they may need to start dialysis within 12-24 months, they are often referred to pre-dialysis multidisciplinary clinics located within a hospital setting, housed only at a regional renal program. Within the pre-dialysis clinic, in order to qualify for ORN funding, the patient must see any three of the following healthcare professionals: nurse, physician, pharmacist/pharmacy technician, dietician or social worker. This model is characterized by a significant variability in access and referral to pre-dialysis care. Multidisciplinary pre-dialysis clinics are hospital-based despite patients being ambulatory and often asymptomatic. Patients often encounter travel expenses, parking fees and difficulty navigating through a busy and complicated hospital setting [7]. A shift to hospital-based care often leads to a disassociation with their primary care practitioner as well. There may be a reluctance to attend hospital-based clinics for asymptomatic patients who prefer to seek their care within the community. The transfer of care from a community-based setting into a hospital-based setting may disrupt continuity of nephrology care for the patient at a critical time in their CKD progression. Continuity of care has been associated with positive outcomes and patient experience [6]. These factors can lead to nonattendance to clinic visits within the hospital setting.
Alternative community-based patient-centred model of care
The alternative community-based, patient-centred care model will provide coordinated care that will optimize access and management of CKD. The aim is to improve attendance, compliance to therapies, and promote a wellness model of care using an experienced RN case manager. This community based model will improve access to multispecialty and multidisciplinary care that already exists within the community for patients with CKD without the need for unnecessary hospital services. Featuring in-house solo and group education, internet-based education across all levels of eGFR, dietary counselling and information sheets, and collaboration with community based pharmacies for medication reviews with availability of on-site laboratory sampling. The advantage of housing pre-dialysis education in community based clinics results in earlier access to education, continuous care throughout disease progression and improved access (not all patients live close enough to hospitals to access hospital based programs). Community based pre-dialysis care models can deliver care equivalent to hospital based programs in a more patient centred and cost effective manner.
In the alternative model of renal care, traditional care will continue in addition to the use of internet based technology across all levels of eGFR to enhance patient education along with strategies to improve access to care in the community. Our assumption is that improving access in the community will lead to improved patient compliance and attendance with fewer patients lost to follow up. The goals of the community-based model are: improved access, continuity of care, enhanced compliance and attendance, fostering further innovation and on-going research.
Results and Discussion
Education and access
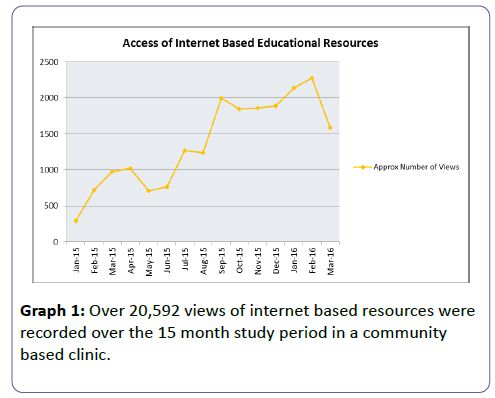
The use of web based education increases access for patients and has already proven to be effective with mass public education campaigns. A strong focus on early, convenient and accessible education across all levels of eGFR was maintained within the community clinic (Graph 1).
Internet based education was utilized in conjunction with one on one or group education by an experienced RN case manager. During the study period over 20,592 views of internet based resources were recorded with increasing frequency.
Our findings suggest that patient education is the most important part of multidisciplinary care and that using available technology in conjunction with in person education can be an effective way to deliver education in a patient centred and cost effective way.
Optimal vs. suboptimal starts
Optimal starts were defined as planned starts with the access most suitable for the patient i.e., by arteriovenous fistula (AVF), peritoneal (PD) catheter or by a central venous catheter (CVC) where the patient does not qualify for either AVF or PD.
Suboptimal starts were defined as unplanned starts using a CVC access. Crash starts were identified as anyone who was not followed by a nephrologist prior to starting dialysis and were excluded from analysis.
Optimal and suboptimal start rates
142 dialysis starts were identified and examined within the 15 month study period.
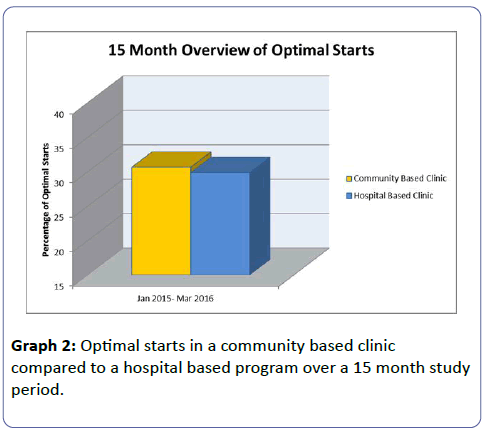
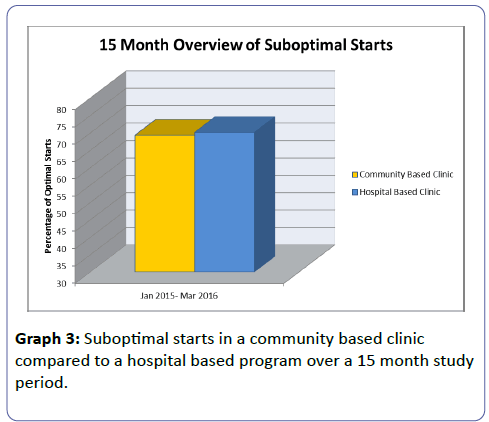
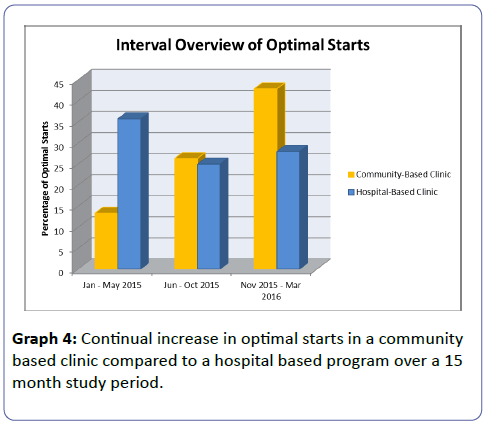
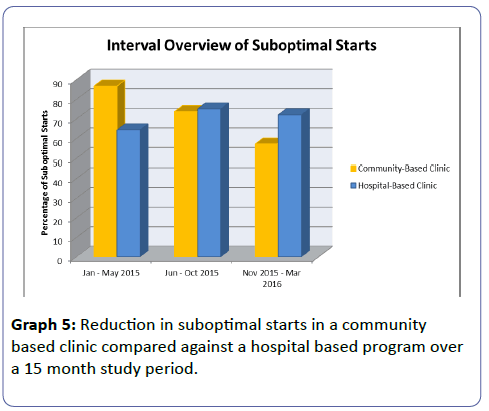
There was a positive correlation between the rates of education and the rates of optimal starts. Although, the overall rates of optimal starts are similar between the community and hospital based clinics; and throughout the study period optimal starts significantly improved for the community based clinics. Between January and May 2015 optimal start rates were 13%, from June to October 2015 they increased to 26% and from November 2015 to March 2016 were up to 43%.
Although not all suboptimal starts can be avoided due to patient decision delays, etc. the implementation of continuous care, early education and increased access in a community based model can minimize suboptimal starts and maximize optimal starts translating to improved quality of life and patient outcomes (Graphs 2-5).
Patient lab value comparisons
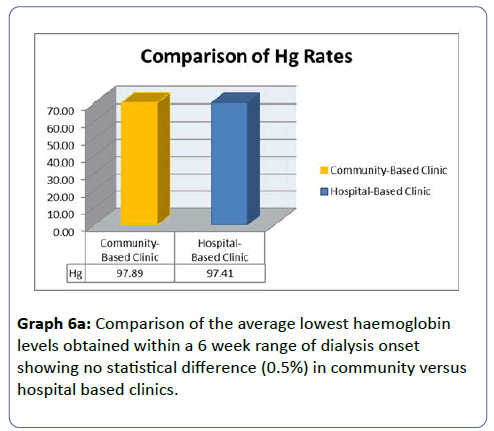
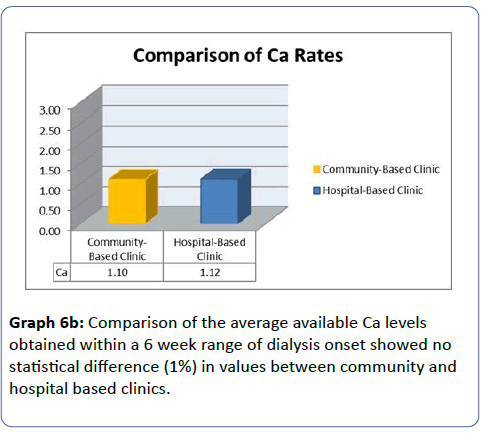
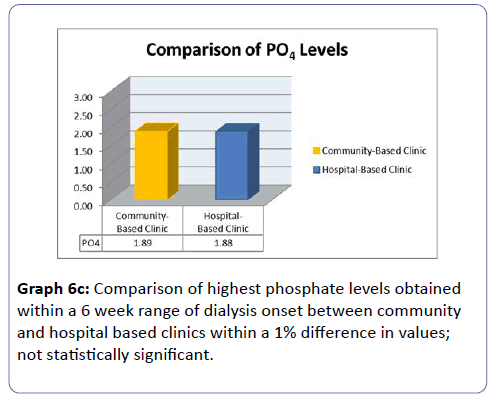
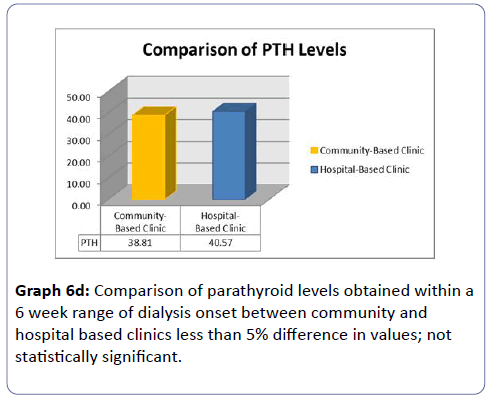
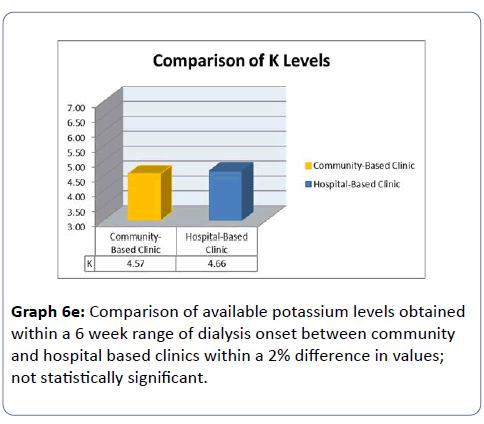
A comparison of the average labs values (Hg, Ca, PO4, PTH, K) of newly started dialysis patients was performed on patients in the 15 month study period to compare community and hospital based clinics. Average values were obtained within 6 weeks of start date, at start date, or as soon after start where possible.
Lab values: haemoglobin levels
The average lowest haemoglobin levels showed 0.5% difference, available calcium levels had 1% difference, phosphate levels were <1%, parathyroid hormone levels were <4.5% and potassium levels showed approximately a 2% difference between community and hospital-based programs. The comparison showed no statistical significance in the difference between these values indicating care was consistent (Graphs 6a-6e).
Calcium levels
PO4 levels
Parathyroid hormone levels
Potassium levels
Non-attendance rates and patient compliance
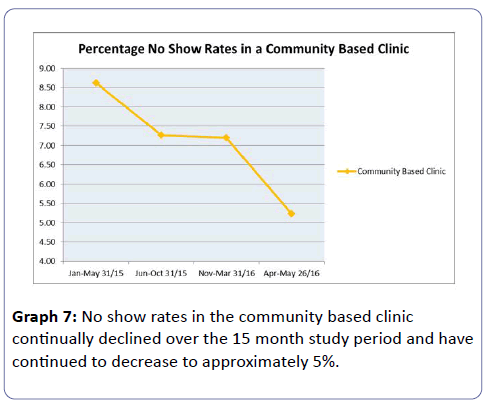
Patient satisfaction is associated with attendance, thus non-attendance show rates are a good indicator in this regard. The non-attendance rates were examined over 5 month intervals throughout the study period. Patients who rescheduled their appointments the day of or were no-shows were counted as non-attendance. The average non-attendance rates were 8.62%, 7.27%, and 7.2%, showing a declining trend. Following the study period and to date the average no show rate has decreased to 5.23% (Graph 7).
Comparison of lab values in new dialysis patients: patient satisfaction
In our past experience hospital non-attendance rates in similarly structured clinics were much higher. Community based outpatient models likely have lower non-attendance rates due to the wellness culture afforded to being outside of the hospital system. A model of wellness promotes not only attendance but patient compliance to proven therapies. This enhances the ability to provide a more continuous model of care, with the hopes of losing fewer patients to follow up who could end up with crash or suboptimal starts on dialysis and relying more frequently on emergency room visits.
A 15-month retrospective study of a community based CKD clinic utilizing components of a novel model of care and a focus on innovation, algorithmic care, education, patient attendance and cost effectiveness was examined between Jan 2015 and March 2016.
It can be difficult to deliver full multidisciplinary care practically on patients due to long wait times in clinic, increased parking fees and managing flow in clinics. In fact, our experience with multidisciplinary care from 2003 to 2013 showed that many patients did not receive care that met definitions due to a variety of factors. This illustrated the need to adopt a more patient centred approach. An innovative community based model of care that utilized an experienced RN case manager to ensure education was accessible and access was timely. To allow flexibility of scheduling for patients, pre-dialysis patients with eGFR<30 were mixed in with general nephrology clinics. In past experience within hospital based clinics with a similar scheduling model, non-attendance rates were above desired targets.
Cost effectiveness
Patients within the community based clinic received no funding for their care. Patients within the hospital based model received funding from the ORN. According to funding formulas during this time period, each patient enrolled in a hospital based CKD pre-dialysis clinic received $1383/patient/calendar year. Estimated cost savings between January 1, 2015 and March 31, 2016 was between $1.5–1.8 million based on patient eligibility criteria and funding formulas during that time.
During the study period patients eligible for funding were provided care in the community in absence of any funding. This community model translated into an estimated taxpayer savings of approximately 1.5-1.8 million dollars ($1383/patient/yr, eGFR<30) over the 15 month study period was calculated based on the 2013/14 CKD Funding Guide, pre-dialysis bundle payments [7]. Not only were tax dollars saved in the community model but simultaneously target outcome indicators improved: optimal start rates increased and no show rates declined. The availability of existing hospital based funding for these patients within a community based model accountable to measurable outcome indicators would continue to allow for expansion of components of the model.
Conclusion
Innovation and research is definitely needed within the CKD population to finds ways to provide community based patient centred care that is cost-effective. Previous data supporting the effectiveness of MDC care has made comparisons to usual nephrology care but not examined novel ways to deliver this care in the community. The various components of this type of care are already being delivered effectively in many communities. Levin et al. concluded that there is a lack of randomized trial data to inform care and there have been no standardized definitions or structure of CKD clinics, nor any metrics by which to evaluate these clinics within nephrology communities. They also concluded that further research is needed to understand how CKD clinic structure/model of care influences patient care and outcomes [8]. In this community based model with continuous implementation of components of the model alongside continuous quality improvement over 15 month period there has been a substantial increase in access to education, a decline in no show rates, and overall reduction in suboptimal starts. Our findings suggest that patient education is the most important part of multidisciplinary care and that using available technology in conjunction with in person education can be an effective way to deliver care in a patient centred and cost effective way. It is important to consider that our novel model of care is in its infancy and is in evolution with room to improve with additional features and community-based connections and communication initiatives. Standard MDC care has been in place for many years; growth is relatively static and is not likely to allow for significant improvements from a chronic baseline. Johns et al. concluded that although interdisciplinary care clinics appear promising in CKD care, studies with longer follow-up and higher risk patients are required to better understand the quality and utility of these clinics and that robust studies regarding the cost-effectiveness of these clinics should be pursued, planned and performed [9]. A community based model of care would like be more effective at promoting an attitude of wellness, be beneficial to those in rural areas and to those patients who prefer to avoid a hospital atmosphere and may allow for better co-ordination of community based care from other specialists and primary care practitioners. Future follow up studies, particularly randomized control trials could examine the effects on ER visits, rates of HD, cardio renal syndrome, and hospital admissions. A prospective RCT comparing community based to hospital-based pre-dialysis clinics with equal resources would best evaluate the difference between a community-based comprehensive multidisciplinary care models with a focus on vascular preventative strategies compared to standard care models [10].
Disclosures
This research received no financial incentives or funding.
Acknowledgements
With appreciation to Ontario Renal Network and Erie St. Clair Local Health Integration Network for their support of our vision to bring Windsor and Essex County the first regional Vascular Health and Research Institute, centre of excellence in cardiovascular and renal disease prevention. We would like to acknowledge Amina Ibrahim and Alia Ibrahim from the University of Windsor Biological Sciences Program for their help in preparing the final draft of this paper.
References
- Canadian Society of Nephrology, The Kidney Foundation of Canada (2014) Developing a Canadian research strategy in pre-dialysis Chronic Kidney Disease.
- Ontario Renal Network. Revised Pre-Dialysis Clinic Eligibility Criteria.
- 2013/14 Chronic Kidney Disease (CKD) (2013) Funding Guide: Version 2.0 Ontario Renal Network.
- Mehdelssohn DC (2008) Predialysis Care: Challenges and Opportunities.
- LHIN, ORN (2014) Letters of support.
- Health Quality Ontario (2013) Continuity of care to optimize chronic disease management in the community setting: an evidence-based analysis. Ont Health Technol Assess Ser 13: 1–41.
- Chronic Kidney Disease (CKD) Funding Guide (2013) Version 2.0 Ontario Renal Network.
- Levin A, Steven S, Selina A, Flora A, Sarah G, et al. (2014) Canadian chronic kidney disease clinics: a national survey of structure, function and models of care. Can J Kidney Health Dis 1: 29.
- Johns, TS, Yee J, Smith-Jules T, Campbell, RC, Bauer C (2015) Interdisciplinary care clinics in chronic kidney disease. BMC Nephrol 16: 161.
- Kadri (2016) An Innovative Model of Care for Vascular Health.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences