Automated Peritoneal Dialysis-related Peritonitis Caused by Morganella Morganii: A Case Report with Review of Relevant Literature
Kyeong Min Kim, Jong Ho Shin, Jin Uk Jeong and Kitae Bang
DOI10.21767/2472-5056.100049
Kyeong Min Kim, Jong Ho Shin, Jin Uk Jeong and Kitae Bang*
Eulji University Hospital, Republic of Korea
- *Corresponding Author:
- Kitae Bang
Eulji University Hospital, Republic of Korea
Tel: 821030038934
E-mail: starryroom@hanmail.net
Received date: October 25, 2017; Accepted date: November 01, 2017; Published date: November 03, 2017
Citation: Kim KM, Shin JH, Jeong JU, Bang K (2017) Automated Peritoneal Dialysis-related Peritonitis Caused by Morganella Morganii: A Case Report with Review of Relevant Literature. J Clin Exp Nephrol Vol.2:49. doi: 10.21767/2472-5056.100049
Copyright: © 2017 Kim KM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Morganella morganii (M. Morganii) is a Gram-negative rod that is part of the normal flora in humans. However, M. Morganii is a rare cause of PD-related peritonitis. A 78-year-old woman with end-stage renal disease secondary to diabetes mellitus on Automated Peritoneal Dialysis (PD) admitted with abdominal pain and cloudy peritoneal fluid. After performing a peritoneal fluid culture, the patient was treated with intraperitoneal (IP) antibiotics. On hospital day 4, a culture of the peritoneal fluid revealed M. Morgani. Although IP antibiotics injection had lasted in the home, however, on 9th day after discharge, effluent peritoneal fluid became cloudy again. Further laboratory tests showed an elevated peritoneal WBC count. We considered the antibiotic treatment to have failed due to bacterial colonization of the surface of the peritoneal Tenckhoff catheter. Therefore, we decided to remove the catheter, and switch the treatment regimen to haemodialysis. Subsequent intraperitoneal cultures were identified as M. Morganii with the same sensitivity as before. Our patient may be first case of PD related peritonitis by M. morganii in Republic of Korea.
Keywords
Peritoneal dialysis; Peritonitis; Dialysis; Morganella morganii
Introduction
Peritoneal dialysis (PD)-related infection is the most common and serious complication in patients undergoing continuous ambulatory peritoneal dialysis (CAPD) or automated peritoneal dialysis (APD). Morganella morganii (M. Morganii) is a species of Gram-negative rod that is part of the normal flora of the intestinal tract in humans and mammals, and reptiles. It is considered an uncommon cause of community-acquired infection and a rare cause of PD-related peritonitis [1]. So far reported in literature, this case is the first report of PD-related peritonitis caused by M. morganii in Republic of Korea. Here we report a case of M. Morganii in a patient with peritonitis with review of relevant literature.
Case Report
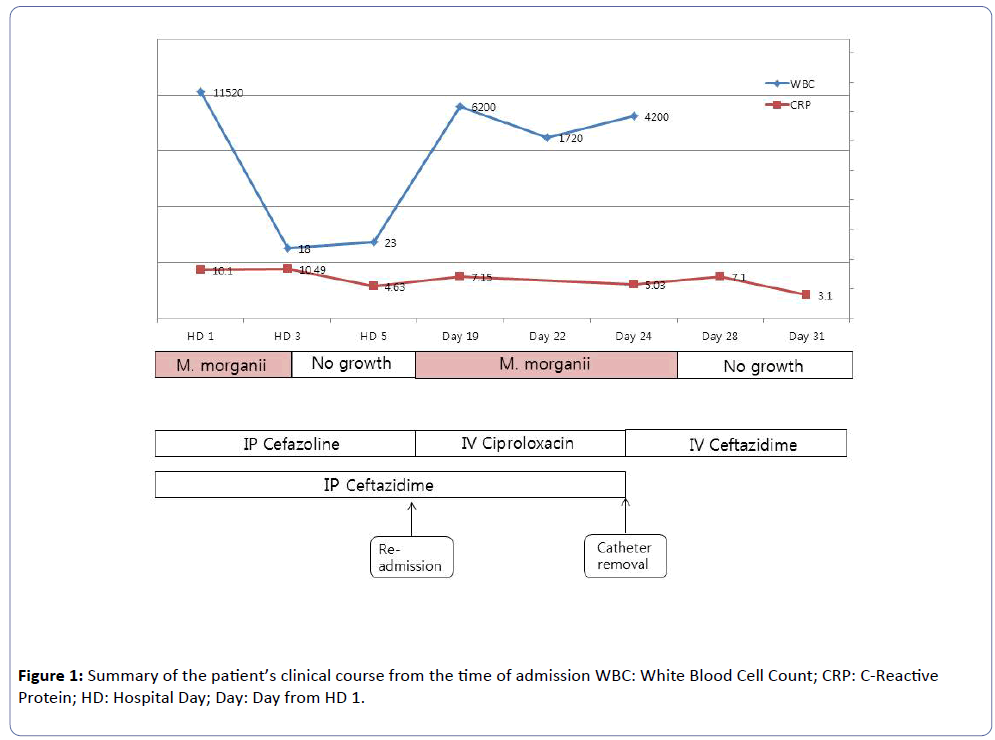
A 78-year-old woman with end-stage renal disease secondary to diabetes mellitus on APD was admitted because of abdominal pain and cloudy peritoneal fluid. Five years prior to admission, CAPD was initiated for end-stage renal disease and switched to APD three years before. Upon physical examination, her blood pressure was 130/70 mmHg, her heart rate was 88 beats/min, her respiratory rate was 16 breaths/ min and; her temperature was 37.6°C. A laboratory investigation revealed the following findings: haemoglobin (Hb)=9.9 g/dL; white blood cell count (WBC)=9,490/mm3 with 82% polymorphonuclear cells; C-reactive protein (CRP)=10.1mg/dL; and liver enzymes were normal. A physical examination revealed a remarkable level of abdominal tenderness. The exit of the peritoneal dialysis catheter looked clean, without any apparent signs of tunnel infection. The effluent peritoneal fluid was cloudy, with a WBC count of 11,500/mm3 (predominantly polymorphonuclear cells). Based on the results of the peritoneal fluid culture, the patient was treated with intraperitoneal (IP) antibiotics, specifically cefazolin 1 gram and ceftazidime 1 gram. Two days after the start of the antibiotic therapy, the patient’s abdominal pain subsided and the peritoneal fluid became clear. On five at the hospital, a culture of the peritoneal fluid obtained on admission day revealed M. Morganii which was sensitive to ciprofloxacin, ceftazidime and piperacillin/tazobactam and resistant to cefazolin and amoxicillin. As a result, the antibiotic regimen was switched to IP ceftazidime alone. A subsequent peritoneal fluid culture obtained on day five at the hospital, was free of organisms; therefore, treatment with IP ceftazidime was continued, and the patient was discharged on the six day after admission. Although IP antibiotics were administered regularly at home, on ninth day after discharge, the patient’s effluent peritoneal fluid became cloudy again. Further laboratory tests showed an elevated CRP level, leucocytosis and peritoneal WBC count. We considered the antibiotic treatment to have failed due to bacterial colonization of the surface of the peritoneal Tenckhoff catheter. Therefore, we decided to remove the catheter, and switch the treatment regimen to haemodialysis. Subsequent intraperitoneal cultures were identified as M. Morganii with the same sensitivity as before. The IP antibiotics were discontinued and ceftazidime was administered intravenously for an additional two weeks, while the patient continued to remain asymptomatic. In addition, the peritoneal WBC count decreased to less than 100/mm3, without dominance of polymorphonuclear cells (Figure 1).
To rule out diverticulosis, a colonoscopy was done after the removal of the catheter, which showed normal colonoscopy findings without any diverticuli. No recurrence of abdominal signs or symptoms was noted during the subsequent two months of follow-up.
Discussion
M. morganii was first described by a British bacteriologist H. de R. Morgan in 1906 as Morgan's bacillus. Initially, M. morganii had been classified in the Proteus genus, and had been called Proteus morganii. In 1978, however it was reclassified into the Morganella genus [2]. M. morganii has been reported to be the cause of urinary tract infections, arthritis, pericarditis, pyomyositis, sepsis, chorioamnionitis, ecthyma gangrenosum-like eruptions, meningitis, renal abscesses, and gas gangrene in neonates or elderly immunocompromised patients or in those with other serious underlying diseases. M. morganii infections generally respond well to appropriate antimicrobial chemotherapy; however, Morganella species are capable of producing β-lactamases and organism’s natural resistance to many β-lactam antimicrobial agents may lead to delays in proper and effective treatment [3]. M. morganii produces urease, which generates ammonia from urea, and is associated with crystalline bacterial biofilm formation on urinary catheters [4].
Peritonitis is a common complication in patients who are on both CAPD and APD. Multicenter studies and registry data analyses tend to show similar peritonitis rates between the two modalities [5,6]. Single center studies with a relatively large population that have a standard protocol of management within the center; however, often show lower peritonitis rates in APD compared with those in CAPD [7,8].
The first case of CAPD-related peritonitis caused by M. morganii appeared in Turkey in 2010 [9]. The second case occurred in Taiwan [10], the third case was in Austria [11] and the fourth case was in Japan [12]. This case is the fifth case of PD-related peritonitis caused by M. morganii and the first case of APD related peritonitis caused by M. so far reported in literature. All five patients in these reported cases were treated with IP or IV antibiotics and two patients didn’t undergo catheter removal, however, PD-catheter had been removed in three patients. In three cases, haemodialysis was performed temporarily, and in one case it was changed to haemodialysis without PD- restart (Table 1).
| Ref | Age | Sex | Cause of ESRD | Form of PD | Combined problems | Treatment | Catheter Removal | Outcome |
|---|---|---|---|---|---|---|---|---|
| 9 (1st) | 55 | F | Hypertension | CAPD | Polymicrobial fashion with Providencia Rettgeri | Interim HD IP cefrperazone & vancomycin → IP imipenem & amikacin | X | Cure Re-start CAPD |
| 10 (2nd) | 62 | F | Hypertension | CAPD | Two months after Prevotella species peritonitis | IV cefmetazole →IP ceftazidime | X | Cure |
| 11 (3rd) | 53 | M | IgA nephropathy | CAPD | Dverticulitis | Interim HD IP vancomycin, Ceftazidime | O | Cure Re-start CAPD |
| 12 (4th) | 68 | M | Hypertension | CAPD | Diverticulosis | Interim HD IP cefazolin, ceftazidime → IP ceftazidime | O | Cure Conversion to HD |
| This case (5th) | 78 | F | Diabetes Mellitus | APD | Interim HD IP cefazoline, ceftazidime → IV ceftazidime + Ciprofloxacin → IV ceftazidime | O | Cure Re-start APD |
Table 1: A Case of Peritoneal Dialysis- Related Peritonitis Associated with Morganella morganii Reported in the Literature.
In the third and fourth cases mentioned above, the authors emphasized that if a patient had multiple diverticula, which is a weak portion of bacterial penetration, and it induces recurrent peritonitis, then the catheters should be explanted. Therefore, in this case, we performed colonoscopy, but the present patient showed normal colonoscopy finding without any diverticuli.
Conclusion
M. Morganii is a rare cause of PD-related peritonitis, and our patient may be first report of PD-related peritonitis caused by M. morganii.
References
- Falagas ME, Kavvadia PK, Mantadakis E, Kofteridis DP, Bliziotis IA, et al. (2006) Morganella morganii infections in a tertiary general hospital. Infection 34: 315–321.
- O’Hara CM, Brenner FW, Miller JM (2000) Classification, identification, and clinical significance of Proteus, Providencia ,and Morganella. Clin Microbiol Rev 13: 534-546.
- Pitout JD, Sanders CC, Sanders WE Jr (1997) Antimicrobial resistance with focus on β-lactam resistance in gram-negative bacilli. Am J Med 103: 51-59.
- Stickler D, Morris N, Moreno MC, Sabbuba N (1998) Studies on the formation of crystalline bacterial biofilms on urethral catheters. Eur J Cin Microbiol Infect Dis 17: 649-652.
- Huang JW, Hung KY, Yen CJ, Huang JW, Hung KY, et al. (2001) Comparison of infectious complications in peritoneal dialysis patients using either a twin-bag system or automated peritoneal dialysis. Nephrol Dial Transplant 16: 604–607.
- Ghali JR, Bannister KM, Brown FG, Rosman JB, Wiggins KJ, et al. (2011) Microbiology and outcomes of peritonitis in Australian peritoneal dialysis patients. Perit Dial Int 31: 651–662.
- El-Reshaid, Wael, Hanan Al-disawy, Hossameldeen Nassef, Usama Alhelaly (2016) Comparison of peritonitis rates and patient survival in automated and continuous ambulatory peritoneal dialysis: a 10-year single center experience. Ren Fail 38: 1187–1192.
- S anchez AR, Madonia C, Rascon-Pacheco RA (2008) Improved patient/technique survival and peritonitis rates in patients treated with automated peritoneal dialysis when compared to continuous ambulatory peritoneal dialysis in a Mexican PD center. Kidney Int Suppl 108: S76–80.
- A talay H, Güney I, Solak Y, Almaz E (2010) First case of CAPD-related peritonitis caused by Morganella morganii. Perit Dial Int 30: 119–121.
- Tsai MT, Yeh JT, Yang WC, Wu TH (2013) CAPD-related peritonitis caused by Morganella morganii. Perit Dial Int 33: 104-105.
- Windpessl M, Prammer W, Asböck R, Wallner M (2013) More on peritonitis by Morganella morganii. Perit Dial Int 33: 467-468.
- Kimura, Yukihiro, Ayano Ito, Kanyu Miyamoto, Norihiro Suga, et al. (2016) Morganella Morganii Peritonitis Associated with Continuous Ambulatory Peritoneal Dialysis (CAPD) after Colonoscopy. Internal Medicine 55: 165–168.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences