Ambulatory Atherosclerotic Index (AASI) and Pulse Pressure (PP) Predicts Hypertension-Induced Renal Vascular Damage
Yuanyuan Gao
Department of Geriatrics, Capital Medical University, Beijing, China
Published Date: 2024-05-27DOI10.36648/2472-5056.9.3.250
Yuanyuan Gao1*, Yuanping Hou1 and Shuo Li2
1Department of Geriatrics, Capital Medical University, Beijing, China
2Department of Ultrasound Medicine, Capital Medical University, Beijing, China
- *Corresponding Author:
- Yuanyuan Gao
Department of Geriatrics, Capital Medical University, Beijing,
China,
E-mail: gaoyuanyuan1100@gmail.com
Received date: April 25, 2024, Manuscript No. IPJCEN-24-18973; Editor assigned date: April 29, 2024, PreQC No. IPJCEN-24-18973 (PQ); Reviewed date: May 13, 2024, QC No. IPJCEN-24-18973; Revised date: May 20, 2024, Manuscript No. IPJCEN-24-18973 (R); Published date: May 27, 2024, DOI: 10.36648/2472-5056.9.3.250
Citation: Gao Y, Hou Y, Li S (2024) Ambulatory Atherosclerotic Index (AASI) and Pulse Pressure (PP) Predicts Hypertension-Induced Renal Vascular Damage. J Clin Exp Nephrol Vol.9 No.3: 250.
Abstract
This study explores the relationship between intrarenal arterial Resistance Index (RI) and two independent indicators, the Ambulatory Atherosclerotic Index (AASI) and Pulse Pressure (PP), to assess renal vascular damage in hypertensive patients. In light of the 2023 hypertension guidelines advocating for out-of-office blood pressure monitoring, this research investigates the utility of AASI and PP as markers for early vascular deterioration. A total of 1,219 hypertensive patients were analyzed, revealing significant differences in RI, AASI and PP among groups. Pearson's correlation analysis demonstrated a moderate positive correlation between RI and AASI/PP, while Receiver Operating Characteristic (ROC) analysis revealed their effectiveness in predicting renal artery stenosis in elderly hypertensive patients. These findings underscore the potential of RI, AASI and PP as non-invasive tools for the early detection and management of renal vascular damage in hypertensive individuals, offering valuable insights for clinical practice and hypertension management.
Keywords
Blood pressure; Hypertension; Resistance Index (RI); Pulse pressure
Introduction
Hypertension, characterized by elevated blood pressure, remains a significant global health concern, with a growing body of research dedicated to understanding its complexities and implications. The 17th Eastern Cardiology Conference (ECC 2023) recently released the 2023 guidelines for managing hypertension, introducing novel diagnostic criteria that include out-of-office blood pressure monitoring [1,2]. These guidelines underscore the importance of accurate blood pressure assessment, emphasizing the use of 24 hrs Ambulatory Blood Pressure Monitoring (ABPM) to provide a more comprehensive evaluation of blood pressure patterns compared to in-office results [2].
Out-of-office blood pressure monitoring, as advocated by the updated guidelines, encompasses various approaches, such as 24 hrs Ambulatory Blood Pressure Monitoring (ABPM) and home blood pressure monitoring [1,2]. This shift in diagnostic criteria acknowledges the limitations of traditional in-office measurements and reflects the evolving understanding that blood pressure varies throughout the day and night. In-office blood pressure readings may not capture the dynamic nature of blood pressure, potentially leading to misdiagnosis or inadequate risk assessment [2].
Within blood pressure monitoring, recent research has highlighted the significance of two independent indicators: Ambulatory Atherosclerotic Index (AASI) and Pulse Pressure (PP) in early detection of vascular deterioration [3]. AASI, derived from 24 hrs ABPM, has emerged as a valuable non-invasive index for assessing arterial function. Studies have demonstrated that AASI is closely associated with the extent of vascular damage in hypertensive patients and can be used to predict the prognosis of cardiovascular events [3]. PP, on the other hand, represents the difference between systolic and diastolic blood pressure and has been identified as a predictor of overall cardiovascular disease, myocardial infarction, coronary heart disease and heart failure. Together, AASI and PP offer insights into the cardiovascular risk profile of hypertensive individuals beyond traditional blood pressure measurements.
Around two thirds of patients with essential hypertension have abnormal renal vasoregulation at early stages of the disease [4-6]. Renal vascular damage is a well-recognized complication of hypertension that warrants particular attention. Hypertensive patients often exhibit mild to moderate abnormalities in the small renal arteries and microarteries. A significant proportion of these individuals experience early-stage alterations in renal vasoregulation, resulting in reduced renal blood flow due to microarterial constriction. Previous research efforts have focused on assessing the relationship between renal blood flow and renal damage in hypertension. However, these studies often used limited blood flow parameters and primarily explored the correlation with renal function markers like glomerular filtration rate and serum creatinine levels, which may not capture the earliest stages of renal damage.
Renal artery Resistance Index (RI) and renal artery ultrasound have emerged as promising indicators in assessing renal vascular health and predicting cardiovascular outcomes in hypertensive patients. Renal artery ultrasound is a valuable non-invasive tool for assessing renal hemodynamics and detecting renal artery stenosis. Studies have shown that renal artery ultrasound can accurately identify renal artery stenosis, a common complication of hypertension [7]. Furthermore, the severity of renal artery stenosis detected by ultrasound has been correlated with the risk of adverse renal and cardiovascular outcomes, providing important prognostic information for patient management [8]. Worsening of renal function over time is often accompanied by an increased risk of cardiovascular events and mortality, highlighting the prognostic significance of RI and renal artery ultrasound in hypertensive patients [9]. Therefore, the measurement of hemodynamic changes in renal arteries with color Doppler ultrasound is of great significance for hypertension patients in capturing early signs of hypertension-induced vascular damage.
There is a clear need to identify the role of AASI and PP in predicting cardiovascular outcomes and identifying patients at risk of renal artery stenosis. This study aims to bridge these knowledge gaps by examining the correlation between intrarenal arterial Resistance Index (RI), AASI and PP, thereby shedding light on the extent of renal vascular damage in hypertensive individuals.
Materials and Methods
Study population
A cohort study of 1,226 hypertensive patients was selected from our department between May 2018 and May 2023. This included 78 patients with renal artery hemodynamic abnormalities (experimental group 1), 1,039 patients with normal renal hemodynamics (control group), and 109 patients with renal artery hemodynamic abnormalities but without renal artery stenosis (experimental group 2). Demographic details shown in Table 1.
| Group | Total | Male | Female | Age range | Age mean |
|---|---|---|---|---|---|
| Experimental group 1 (with definite renal artery stenosis) | 78 | 32 | 46 | 50-82 | 73.7 ± 5 |
| Experimental group 2 (without renal artery stenosis | 109 | 63 | 46 | 50-78 | 57 ± 15 |
| All cases with renal artery hemodynamic abnormality hypertension | 187 | 95 | 92 | 50-82 | 64.7 ± 16 |
| Control group | 1039 | 546 | 493 | 50-78 | 59 ± 16 |
Table 1: Demographic details of all experimental groups included in the study.
Inclusion criteria: Inclusion criteria encompassed patients (1) Graded and determined according to the 2023 guidelines for hypertension management [10]; (2) Hypertension wellcontrolled under medication; (3) Renal hemodynamic abnormality [11]; renal artery resistance index greater than 0.75; (4) Renal artery stenosis [12]; and renal arteriography.
Exclusion criteria: (1) Secondary hypertension; (2) Diabetes mellitus and primary renal disease. (3) Imperfect examination results. Signed informed consent was obtained from all participants and the study protocol was approved by the Medical Ethics Committee of Beijing Chaoyang Hospital (approval file No. 2021-Ke-704).
Renal blood flow measurement
Renal blood flow was assessed using color ultrasound diagnostic instruments (GE LOGIQ E9, Myeri ResonaR9) with a probe frequency of 2-4 MHz, a sampling volume of 1-2 mm and an angle of <60 degrees of blood flow sound velocity. All subjects were fasted and dehydrated and placed in the left and right lateral positions, operated by the same physician to display the color blood flow signals in the long axis of the kidney and the intrarenal vascular bed. The blood flow spectra of the left and right main renal artery, lobar segmental artery and middle lobar artery, the Peak Systolic flow Velocity (PSV), the End-Diastolic flow Velocity (EDV) and the RI of each level of arteries = (PSVEDV/ PSV) were taken respectively and each index was measured continuously for more than three cardiac cycles with averages taken.
The diagnostic criteria for renal hemodynamic abnormalities are: Peak systolic flow velocity at the stenosis site greater than 180 cm/s, the ratio of peak systolic flow velocity in the abdominal aorta at the renal artery to renal artery level is above 3.5 and acceleration time after stenosis >0.07 s and early systolic acceleration <300 cm/s, with a difference in RI between renal artery trunk and segmental artery >0.15.
The criteria for renal artery stenosis (>60%) are:
• Peak Systolic Velocity (PSV) ≥ 180 cm/sec, with turbulent flow after stenosis
• The ratio of renal artery to abdominal aorta PSV is ≥ 3.5
• RI>0.8
• Stenosis pressure gradient >20 mmHg indicates renal artery stenosis. If no blood flow spectrum is measured at the renal vessels and the renal diameter is less than 7 cm, the renal artery may be completely occluded.
• This examination is non-invasive, inexpensive, safe and not affected by renal function, making it suitable for screening and follow-up. Renal artery CTA and renal artery angiography are not suitable for the elderly patients mentioned in this article.
Ambulatory blood pressure measurement
Ambulatory blood pressure monitoring was conducted using a non-invasive portable monitor (SunTech, USA) with measurements taken at 0.5 hrs intervals during daytime (6:00-22:00) and 1.0 hrs intervals during nighttime (22:00-6:00). Changes in blood pressure were recorded for 24 hrs and the slope of the regression of the diastolic blood pressure on systolic blood pressure was calculated with the diastolic blood pressure as the longitudinal coordinate and the systolic blood pressure as the horizontal coordinate, and AASI= (1-regression slope). The slope of regression of diastolic blood pressure on systolic blood pressure was determined by taking diastolic blood pressure as the vertical coordinate and systolic blood pressure as the horizontal coordinate.
Observation indexes include: (1) Comparison of AASI and PP of hypertensive patients with different degrees of increased renal blood flow resistance; (2) Spearman rank sum correlation analysis used to evaluate the correlation between AASI, PP and the degree of renal injury in elderly hypertensive patients; and (3) Receiver Operating Characteristic (ROC) curve analysis of the presence or absence of renal artery stenosis and the results of RI, AASI and PP in hypertensive patients with abnormal renal hemodynamics.
Statistical analysis
Data were analyzed using SPSS 26.0 software. Measurement data were expressed as (x ± s), t-test for two-by-two comparisons, and chi-square test for multi-group comparisons; count data were expressed as (%) and χ2 test was performed for inter-group comparisons; correlations were performed by Pearson correlation analysis; the ROC curve was used to analyze the predictive value of RI, AASI and PP for hypertension combined with renal stenosis in the elderly; P<0.05 was considered as statistically significant. ROC curve was used to analyze the predictive value of RI, AASI and PP for hypertension and renal artery stenosis in the elderly.
Results
Comparison of parameters among groups
Significant differences were observed in RI, AASI and PP among the three groups (experimental group 1, experimental group 2 and control group). Specifically, the mean RI was 0.83 ± 0.05 in experimental group 1, 0.78 ± 0.02 in experimental group 2 and 0.71 ± 0.03 in the control group (F=410.436, p<0.001). Similarly, AASI and PP showed statistically significant differences among the groups (F=734.773 and 968.991, respectively, both p<0.001). Further pairwise comparisons revealed significant differences between experimental group 1 and group 2 for all parameters (F=66.337, 9.871 and 160.514 for RI, AASI and PP, respectively; all p<0.05), indicating distinct hemodynamic profiles associated with renal artery stenosis as shown in Table 2.
| Experimental group I | Experimental group II | Control group | Statistical value | P-value | |
|---|---|---|---|---|---|
| RI | 0.83 ± 0.05 | 0.78 ± 0.02 | 0.71 ± 0.03 | 410.44* | <0.001* |
| 66.34** | <0.001** | ||||
| AASI | 0.61 ± 0.05 | 0.58 ± 0.06 | 0.37 ± 0.05 | 734.77* | <0.001* |
| 9.87** | 0.002** | ||||
| PP | 1.71 ± 0.15 | 1.44 ± 0.22 | 0.88 ± 0.25 | 968.99* | <0.001* |
| 160.51** | <0.001** | ||||
| Blood creatinine | 97.66 ± 32.72 | 82.99 ± 18.51 | 78.76 ± 20.75 | 9.898* | <0.001* |
| 15.52** | 0.001** | ||||
| Urine protein | 17.949 ± 2.95 | 7.339 ± 1.36 | 17.949 ± 2.95 | 4.189* | 0.016* |
| 5.210** | 0.024** | ||||
| Note: (*): Comparison between groups; (**): Comparison between two groups of an experimental group. | |||||
Table 2: Comparison of RI, AASI and PP between experimental and control groups.
Logistic regression analysis of renal artery stenosis
Pearson correlation analysis demonstrated a moderate positive correlation between RI and AASI (r=0.730, p<0.001) as well as RI and PP (r=0.762, p<0.001). These findings suggest that higher levels of intrarenal arterial resistance are associated with increased ambulatory atherosclerotic index and pulse pressure, indicating a potential link between renal vascular damage and systemic vascular dysfunction.
Using the occurrence of renal artery stenosis in hypertensive patients as the dependent variable, all factors were transformed into independent variables, i.e. RI, AASI, PP, Blood creativity and urine protein were used as independent variables. Univariate logistic regression analysis showed that all independent variables had statistical differences. Multivariate logistic regression analysis showed that RI, AASI and PP had statistical differences (P<0.05) (Table 3).
| Univariate analysis | Multivariate analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| Coefficients | 95% Confidence interval | P-value | Coefficients | 95% Confidence interval | P-value | |||
| Lower | Upper | Lower | Upper | |||||
| Intercept | -5.636 | -6.613 | -4.66 | <0.001 | ||||
| RI | 6.199 | 4.675 | 7.664 | <0.001 | 3.924 | 2.751 | 5.097 | <0.001 |
| AASI | 1.887 | 0.702 | 3.072 | 0.002 | 0.978 | 0.176 | 1.779 | 0.017 |
| PP | 1.73 | 1.461 | 1.999 | <0.001 | 1.361 | 1.106 | 1.615 | <0.001 |
| Blood creatinine | 0.004 | 0.002 | 0.007 | 0.003 | / | / | / | 0.125 |
| Urine protein | 0.002 | 0 | 0.005 | 0.026 | / | / | / | 0.349 |
Table 3: Results of logistic regression analysis of renal artery stenosis.
Predictive value for renal artery stenosis
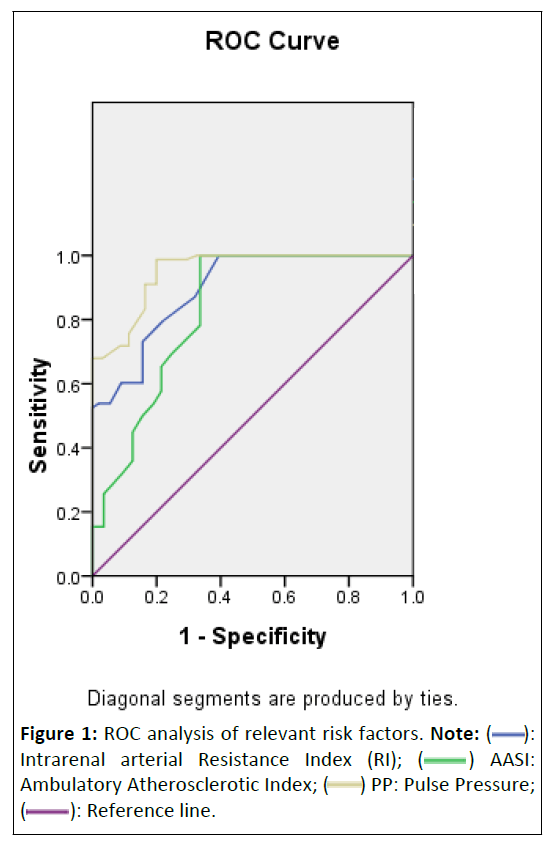
ROC curve analysis was performed to assess the predictive value of RI, AASI and PP for renal artery stenosis in elderly hypertensive patients. The Area Under the Curve (AUC) for RI was 0.897 (95% Confidence Interval (CI) 0.843-0.951), for AASI was 0.830 (95% CI 0.761-0.899) and for PP was 0.951 (95% CI 0.917-0.985), all with statistical significance (p<0.05). The optimal cutoff values for predicting renal artery stenosis were determined as RI=0.77, AASI=0.54 and PP=1.33, with corresponding sensitivities of 87%, 95%, 98% and specificities of 68%, 67% and 71%, respectively. These results underscore the potential of RI, AASI and PP as effective predictors for renal artery stenosis in elderly hypertensive patients (Table 4 and Figure 1).
| Associated risk factors | Truncated value | AUC | Standard error | p-value | 95% confidence interval | Sensitivity | Specificity |
|---|---|---|---|---|---|---|---|
| RI | 0.77 | 0.9 | 0.018 | 0 | 0.86-0.93 | 0.87 | 0.68 |
| AASI | 0.54 | 0.83 | 0.022 | 0 | 0.79-0.87 | 0.95 | 0.67 |
| PP | 1.33 | 0.951 | 0.011 | 0.023 | 0.929-0.972 | 0.98 | 0.71 |
Table 4: Results of ROC curve analysis of relevant risk factors.
Discussion
Renal damage in hypertension is one of the serious complications of hypertension [10,12]. Mild to moderate abnormalities of the small renal arteries and microarteries are common in patients with essential hypertension. Early on, about two thirds of them have abnormal regulation of the renal vasculature and renal blood flow can be reduced due to the constriction of micro arteries [11].
The current study builds upon a growing body of research in hypertension management and vascular damage. Our findings align with previous research emphasizing the importance of outof- office blood pressure monitoring, as outlined in the 2023 guidelines [1-4]. These guidelines acknowledge the limitations of in-office measurements and advocate for the use of 24 hrs Ambulatory Blood Pressure Monitoring (ABPM) to provide a more comprehensive assessment of blood pressure dynamics.
In this study, there were statistically significant differences in between-group comparisons of RI, AASI and PP data (F=410.436, 734.773 and 968.991, P<0.001); and there were statistically significant differences in comparisons of experimental group 1 and group 2 (F=66.337, 9.871 and 160.514, P<0.05). The reasons are analyzed as follows: AASI is a new non-invasive index for assessing arterial function, which is derived from 24 hrs ambulatory blood pressure monitoring and is closely related to the degree of damage to the heart, brain, lungs and other organs in hypertensive patients and can be used to respond to atherosclerosis and predict the prognosis of hypertensive patients. Recently, researchers from leading journals in the field of cardiovascular disease analyzed whether the AASI or PP of 169,613 predicted new-onset cardiovascular disease and death in individuals in a community population. Higher AASI, PP was associated with an increased risk of overall CVD, myocardial infarction, coronary heart disease and heart failure. ASI also predicted death, but PP appeared to be more clinically valuable than AASI.
By Pearson correlation analysis, RI was moderately positively correlated with AASI and PP (r=0.730, 0.762, P<0.001). By ROC analysis, the areas under the curve of RI, AASI and PP for predicting renal artery stenosis in elderly hypertensive patients were 0.897, 0.830 and 0.951 (P<0.05). It is suggested that RI, AASI and PP are closely related to the occurrence and development of renal artery stenosis in hypertensive patients, which should be paid attention to clinically.
In line with previous studies, we found that Ambulatory Atherosclerotic Index (AASI) and Pulse Pressure (PP) are valuable indices for assessing arterial function and predicting cardiovascular outcomes in hypertensive patients. Our study extends this understanding by exploring the relationship between these indices and intrarenal arterial Resistance Index (RI), specifically focusing on renal vascular damage. The moderate positive correlation between RI, AASI and PP observed in our study reinforces the notion that these indices are interconnected and may collectively contribute to the complex pathophysiology of hypertensive vascular damage.
Recent studies have also shown [13] that the correlation between renal blood flow measurements and renal damage in hypertension is still in its infancy. Early studies were mostly focused on the methodological depth of the methodology, using fewer blood flow parameters and in the studies on the relationship with renal function [14-19], the indicators of renal function were limited to the myocardial crisp clearance and blood myocardial crisp levels, which could not represent the earliest stage of renal damage.
The significance of our study lies in its contribution to the refinement of non-invasive tools for assessing renal vascular damage secondary to hypertension. Hypertensive patients frequently experience abnormalities in renal vasoregulation, which may result in reduced renal blood flow due to microarterial constriction [11]. By demonstrating the correlation between RI and AASI and PP, our study underscores the clinical relevance of these indices in identifying early-stage renal vascular damage, potentially enabling timely intervention to mitigate further deterioration.
Furthermore, our study aligns with recent efforts to broaden the utility of AASI and PP beyond cardiovascular risk assessment. While AASI and PP have been established as predictors of cardiovascular events, their application in identifying hypertensive patients at risk of renal artery stenosis is a novel contribution. The ability to use readily available ABPM data to gauge renal vascular health provides a practical and efficient approach for clinicians to enhance their diagnostic and riskstratification capabilities in hypertension management.
Future studies can further explore the clinical utility of RI, AASI and PP in making diagnosis, guiding treatment decisions and predicting outcomes in hypertensive patients, specifically to tailor interventions to the specific vascular needs of individual patients. Whether these indices can predict progression of renal vascular damage and development of renal artery stenosis is also a topic to explore with great clinical significance.
Conclusion
In conclusion, our study highlights the relevance of AASI and PP as non-invasive indices for assessing renal vascular damage in hypertensive patients, complementing traditional blood pressure measurements. By establishing the correlation between these indices and RI, our findings offer valuable insights for clinicians and researchers. Future studies should further validate and expand upon these findings, ultimately enhancing our ability to identify, monitor and manage renal vascular damage in the context of hypertension.
Authors’ Contributions
Conception and design of study, data acquisition, data analysis and interpretation, drafting of manuscript and revision: Yuanyuan Gao.
Acknowledgements
The author extends sincere gratitude to the Department of Geriatrics, Beijing Chaoyang Hospital, Capital Medical University for their valuable support. The author is also deeply thankful to the patients and medical personnel whose participation made this study possible.
References
- Funder JW (2020) Primary aldosteronism: Where are we now? Where to from here? Horm Metab Res 52: 459-466.
[Crossref], [Google Scholar], [Indexed]
- Deussen A, Kopaliani I (2023) Targeting inflammation in hypertension. Curr Opin Nephrol Hypertens 32: 111-117.
[Crossref], [Google Scholar], [Indexed]
- Mitchell BD, Whitlatch HB (2023) Decoding hypertension through primary aldosteronism. Circulation 147: 1110-1111.
[Crossref], [Google Scholar]
- Thomas N (2023) Hypertensive management. Crit Care Nurs Clin North Am 35: 31-38.
[Crossref], [Google Scholar], [Indexed]
- Brown J, Yazdi F, Jodari-Karimi M, Owen JG, Reisin E (2022) Obstructive sleep apnea and hypertension: Updates to a critical relationship. Curr Hypertens Rep 24: 173-184.
[Crossref], [Google Scholar], [Indexed]
- Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, et al. (2018) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension 71: e13–e115.
[Crossref], [Google Scholar], [Indexed]
- Granata A, Fiorini F, Andrulli S, Logias F, Gallieni M, et al. (2009) Doppler ultrasound and renal artery stenosis: An overview. J Ultrasound 12: 133-143.
[Crossref], [Google Scholar], [Indexed]
- Shafique S, Peixoto AJ (2007) Renal artery stenosis and cardiovascular risk. J Clin Hypertens (Greenwich) 9: 201-208.
[Crossref], [Google Scholar], [Indexed]
- Granata A, Zanoli L, Clementi S, Fatuzzo P, Nicolò PD, et al. (2014) Resistive intrarenal index: Myth or reality? Br J Radiol 87: 20140004.
[Crossref], [Google Scholar], [Indexed]
- Pulmonary Function and Clinical Respiratory Physiology Committee of Chinese Association of Chest Physicians (2024) Standard technical specifications for methacholine chloride (Methacholine) bronchial challenge test 2023. Zhonghua Jie He He Hu Xi Za Zhi 47: 101-119.
[Crossref], [Google Scholar], [Indexed]
- Brown JM, Siddiqui M, Calhoun DA, Carey RM, Hopkins PN, et al. (2020) The unrecognized prevalence of primary aldosteronism: A cross-sectional study. Ann Intern Med 173: 10-20.
[Crossref], [Google Scholar], [Indexed]
- Kmieć P, Rosenkranz S, Odenthal M, Caglayan E (2023) Differential role of aldosterone and transforming growth factor beta-1 in cardiac remodeling. Int J Mol Sci 24: 12237.
[Crossref], [Google Scholar], [Indexed]
- Díaz Del Campo LS, García-Redondo AB, Rodríguez C, Zaragoza C, Duro-Sánchez S, et al. (2023) Resolvin D2 attenuates cardiovascular damage in angiotensin II-Induced hypertension. Hypertension 80: 84-96.
[Crossref], [Google Scholar], [Indexed]
- Vaidya A, Carey RM (2020) Evolution of the primary aldosteronism syndrome: Updating the approach. J Clin Endocrinol Metab 105: 3771-3783.
[Crossref], [Google Scholar], [Indexed]
- Drake KM, Ruhm CJ (2023) Estimating drug involvement in fatal overdoses with incomplete information. Am J Prev Med 65: 1172-1180.
[Crossref], [Google Scholar], [Indexed]
- Boos CJ, Toon LT, Almahdi H (2021) The relationship between ambulatory arterial stiffness, inflammation, blood pressure dipping and cardiovascular outcomes. BMC Cardiovasc Disord 21: 139.
[Crossref], [Google Scholar], [Indexed]
- Centers for Disease Control and Prevention (2022) About multiple cause of death, 1999-2020.
- Dong T, Faaborg-Andersen C, Garcia M, Blaha M, Klein AL, et al. (2023) Multimodality cardiovascular imaging in hypertension. Curr Opin Cardiol 38: 287-296.
[Crossref], [Google Scholar], [Indexed]
- Freeman MW, Halvorsen YD, Marshall W, Pater M, Isaacsohn J, et al. (2023) Phase 2 trial of baxdrostat for treatment-resistant hypertension. N Engl J Med 388: 395-405.
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences
 ): Intrarenal arterial Resistance Index (RI); (
): Intrarenal arterial Resistance Index (RI); ( ) AASI: Ambulatory Atherosclerotic Index; (
) AASI: Ambulatory Atherosclerotic Index; ( ) PP: Pulse Pressure; (
) PP: Pulse Pressure; (  ): Reference line.
): Reference line.