Very low doses of direct intravenous iron in each session as maintenance therapy in haemodialysis patients
Javier Deira, Silvia González-Sanchidrián, Santiago Polanco, Clarencio J. Cebrián, María C. Jiménez, Jesús P. Marín, Juan R. Gómez-Martino, Luis Fernández-Pereira and José M. Tabernero
DOI10.21767/2472-5056.100003
Javier Deira1*, Silvia González- Sanchidrián1, Santiago Polanco1, Clarencio J. Cebrián1, María C. Jiménez1, Jesús P. Marín1, Juan R. Gómez-Martino1, Luis Fernández-Pereira2 and José M. Tabernero3
1Department of Internal Medicine, Division of Nephrology, San Pedro de Alcántara Hospital, 10003 Cáceres, Spain
2Service of Clinical Laboratory, Division of Immunology, San Pedro de Alcántara Hospital, 10003 Cáceres, Spain
3Service of Nephrology, Salamanca University Hospital, 37007 Salamanca, Spain
- *Corresponding Author:
- Javier Deira Lorenzo
MD, Department of Internal Medicine, Division of Nephrology
San Pedro de Alcántara Hospital, 10.003 Cáceres, Spain
Tel: 00 34 927 25 62 00
Fax: 00 34 927 25 62 02
E-mail: deiralorenzo@gmail.com
Received date: October 27, 2015 Accepted date: December 17, 2015 Published date: December 21, 2015
Citation: Deira J, González-Sanchidrián S, Polanco S, Cebrián CJ, Jiménez MC, et al. (2015) Very low doses of direct intravenous iron in each session as maintenance therapy in haemodialysis patients. J Clin Exp Nephrol 1:3. DOI: 10.21767/2472-5056.100003
Copyright: © 2015 Deira J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Intravenous (IV) iron supplementation is widely used in haemodialysis (HD) patients to treat their periodic losses. However, the ideal doses and frequency is unknown. We analyse whether treatment with 20 mg of iron IV at the end of each session of HD affects erythropoiesis activity (EA) and functional iron (FI).
Methods: In 36 patients, we measure the reticulocyte count and the content of haemoglobin reticulocyte (CHr) as EA and FI markers respectively, before and four weeks after the end of treatment. Before the study, 23 patients received another different therapy with IV iron as maintenance therapy.
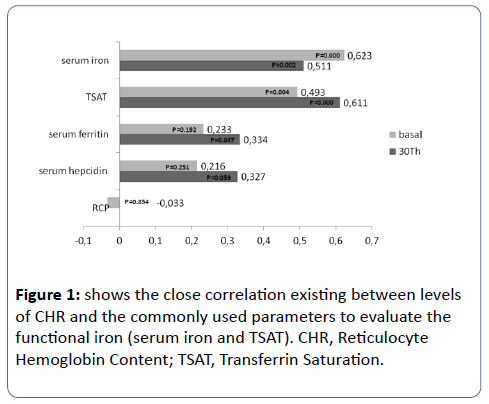
Results: Reticulocyte count was 49.7±23, 8 x103 before and 47.2±17, 2 x103 after the treatment (P=0.51). The CHr was 34.82±3,7 pg and 34.44±3.51 pg respectively (P=0.35), showing an excellent correlation with the others FI markers (serum iron r=0,6 p=0,001; saturation transferrin r=0,49 p=0,004); that is not seen with the serum ferritin (r=0.23 p=0.192) or the hepcidin (r=0.22 p=0.251). The thirteen
patients who did not receive the iron prior the study, showed a high FI levels but not an increase of the serum ferritin or the serum hepcidin.
Conclusions: The administration of a little quantity of iron at the end of every HD session keeps the EA and the FI and allows reducing the iron overload administrated and/or decreasing the iron stores markers in some patients.
Keywords
Anaemia; Erythropoietic Activity; Haemodialysis; Intravenous Iron; Reticulocyte Count.
Abbreviations
CRP-C-Reactive Protein, CHr-Content of Haemoglobin Reticulocyte, EA-Erythropoiesis Activity, ESAs-Erythropoiesis-Stimulating Agents, FI-Functional Iron, FID -Functional Iron Deficiency, HD-Haemodialysis, Htc-Hematocrit, Hb- Hemoglobin, HRC-Hypochromic Red Cells, IV-Intravenous, NTBI-Nontranferrin Bound Iron, RBC-Red Blood Cells, TSAT-Transferrin Saturation
Introduction
Appropriated anaemia management for haemodialysis (HD) patients is changing. Deficiencies of erythropoietin and iron play a role in their genesis, and both must be corrected. Optimal haemoglobin (Hb) target and strategies to balance erythropoiesisstimulating agents (ESAs) and intravenous (IV) iron administration remain unclear [1]. ESAs dose has decreased since recent studies have reported adverse outcomes of effective anaemia correction with ESAs [2-4]. By the otherwise, iron supplementation is widely used in HD patients to treat iron deficiency, prevent its development in ESA-treated, reduce ESAs dose and raise Hb levels in the presence or absence of ESAs treatment, so its use has been increased last year’s [1,5]. However, despite iron supply routine, nephrologists have not yet consensus on several questions: what is the best strategy for iron therapy in dose terms or frequency and if the best way to use iron is administered consistently (i.e. weekly to monthly) or sporadically [6,7]. Also, there is not a consensus in the treatment of anaemia by the functional iron deficiency (FID); in fact, most recently guidelines [8-9] recommend caution with the routine IV iron administration; although, recent studies says that some of those patients may improve with IV iron therapy [10]. Because of that, there is a variation of IV iron therapy in different countries and over the time [11]. In the present paper we report our experience with the administration of 20 mg of IV sucrose iron at the end of every HD session; an unusual maintenance therapy in the clinical practice. We focused in particular on the influence of that kind of maintenance therapy in the erythropoiesis activity (EA) and the functional iron (FI).
Patients and Methods
Analyses were performed in accordance with the Declaration of Helsinki and the guidelines of the institutional review board of the hospital.
All patients of our HD unit were evaluated by this study. Patients who had more than 12 weeks of intermittent HD (3 times a week for 3h-4h) were recruited. Patients that had any kind of infections (defined by the presence of fever or antibiotics treatments) or that received red blood cells transfusion during the study or weeks before and those patients with higher ferritin levels (≥1400 mg/ml) were not included. A total of 36 patients, 13 women and 23 men, were included.
Before starting study, 23 patients received 100 mg of IV sucrose iron diluted in 100 cc of 0.9% saline in the last half an hour of HD, as maintenance therapy. Eight of them once a week, nine every two weeks and six once a month. Thirteen remaining patients not received the iron prior the study. During the study, we administered 20 mg of sucrose iron at the end of every HD session: 1 cc diluted in 10 cc of 0, 9% saline. We infused the iron during one minute using the venous line before the disconnection; as figure in the drug details of the product [12]. Every patient remained in the HD unit for at least 30 minutes after they finished the iron treatment. The patients provided their informed consent.
The study consisted in the basal collection of venous blood samples in the second and fourth week of treatment. The basal data and the data recollected at the end of the study were hematimetria [haemoglobin (Hb), haematocrit (Htc), red blood cells (RBC) and reticulocyte count], and iron status [serum iron, serum transferrin, transferrin saturation (TSAT), serum ferritin, content of haemoglobin reticulocyte (CHr), serum hepcidin and C-Reactive Protein (CRP)]. These determinations were collected one week after the end of iron treatment. In the second week of treatment only hematimetria and CHr were collected without suspension of iron treatment.
The hematimetria and the CHr were measured with a Roche® XE 5000 autoanalyzer. The hepcidin was measured with the DRG® Hepcidin ELISA (EIA-4705 DRG International Inc., USA), a solid phase enzyme-linked immunosorbent assay (this kit is intended for research use only).
Study Objectives
The primary objective of this study was to observe if the administration of 20 mg of sucrose irons in every HD session for four weeks increase the EA (measured by reticulocyte count) and if the FI improve (measured by CHr). Secondary analysis included: the behaviour of those parameters in patients that had been receiving or not iron as a maintenance treatment prior of study; and according with inflammation grade before the study began; as well as the safety and tolerability of this maintenance IV iron treatment.
Data were expressed as mean ± SD. To compare samples between two groups, Student’s t-test was used. Bivariate linear correlations were expressed by Pearson’ correlation coefficients. p less than 0.05 is considered statistically significant.
Results
Iron administration and erythropoiesis
The reticulocyte levels were not significantly affected along the study (Table 1A). Also no correlation was observed between the percentage change in reticulocytes and the rest of parameters studied. At 15 days the Hb, Htc and RBC had a significant descend, but returned to a similar basal levels at the end of the study (Table 1A). In patients that not received iron prior to the study we observed a little increase of erythropoietic parameters (Table 1B). By the other side, in patients that received 100 mg of iron a week as a maintenance treatment we observed a little decrease of such parameters (Table 1C) with not relevant significant difference in both cases.
| Day of Determination | Reticulocytes (absolute nº x 103) | Reticulocytes (%) | Hb (g/dL) |
Hct (%) |
RBC (x106) |
|
|---|---|---|---|---|---|---|
| 1.A Allpatients (n=36) | ||||||
| Basal | 49.7±23.8 | 1.43±0.80 | 10.51±1.46 | 33.01±4.58 | 3.53±0.57 | |
| 15 | 50.7±21.6 | 1.53±0.76 | 10.22±1.65* | 31.98±5.24* | 3.43±0.64* | |
| 30 | 47.2±17.2 | 1.39±0.59 | 10.32±1.97 | 32.68±5.25 | 3.48±0.69 | |
| 1.B Patients that not received the iron prior the study (n=13) | ||||||
| Basal | 52.8±20.3 | 1.55±0.65 | 9.95±1.53 | 31.28±5.25 | 3.40±0.60 | |
| 15 | 56.5±17.5 | 1.69±0.54 | 9.70±1.68 | 30.43±5.76 | 3.32±0.66 | |
| 30 | 53.1±19.3 | 1.53±0.48 | 10.12±1.65 | 31.62±5.78 | 3.42±0.63 | |
| 1.C Patients that received 100 mg/week of iron prior the study (n=8) | ||||||
| Basal | 50.4±27.6 | 1.45±0.94 | 10.59±1.21 | 33.50±3.96 | 3.58±0.54 | |
| 15 | 48.9±22.1 | 1.43±0.72 | 10.37±1.40 | 32.58±4.49 | 3.50±0.59 | |
| 30 | 45.5±16.3 | 1.26±0.46 | 10.37±2.14 | 33.69±4.37 | 3.61±0.55 | |
| Abbreviations: Hb, Hemoglobin; Hct, Hematocrit; RBC, Red Blood Cells. | ||||||
| Abbreviations: Hb, Hemoglobin; Hct, Hematocrit; RBC, Red Blood Cells. * p<0.05 with respect to basal values. |
||||||
Table 1 Results of the Different Erithropoietics Parameters.
Iron administration and iron metabolism
The CHr levels remained practically unaltered throughout the study (Table 2A). In patients that not received iron prior the study we observed a little increase (Table 2B). By the other side, patients that received a 100 mg of iron a week as a maintenance treatment we observed a little decrease of such parameter (Table 2C), with not relevant significant difference in both cases. There was a close correlation between the CHr levels and FI parameters (serum iron and TSAT) at the beginning and the end of the study. This parameter was not correlated in any moment with the serum hepcidin or with the basal CRP (Figure 1).
| Day of Determination | CHr (pg) |
SerumIron (μg/dL) | SerumTransferrin (mg/dL) | TSAT (%) | SerumFerritin (ng/dL) | Hepcidin (ng/mL) |
|---|---|---|---|---|---|---|
| 2.AAllpatients(n=36) | ||||||
| Basal | 34.82±3.71 | 52.87±16.12 | 181.47±36.17 | 24.14±8.59 | 432.91±384.91 | 63.35±36.44 |
| 15 | 34.96±3.07 | |||||
| 30 | 34.44±3.51 | 56.86±21.29 | 186.76±38.41 | 24.71±8.92 | 397.89±309.88 | 65.78±36.42 |
| 2.B Patients that not received the iron prior the study (n=13) | ||||||
| Basal | 33.68±1.48 | 49.31±12.63 | 181.29±31.74 | 21.78±4.44 | 452.26±365.18 | 62.57±37.64 |
| 15 | 33.73±1.9 | |||||
| 30 | 34.27±3.51 | 55.85±21.68 | 186.22±38.403 | 24.69±8.61 | 391.32±279.79 | 58.76±32.53 |
| 2.C Patients that received 100 mg/week of iron prior the study (n=8) | ||||||
| Basal | 34.54±4.26 | 51.25±16.60 | 185.73±32.02 | 22.86±7.96 | 354.22±420.1 | 48.76±35.12 |
| 15 | 34.45±3.63 | |||||
| 30 | 33.63±3.71 | 52.50±21.09 | 191.34±36.15 | 22.26±8.37 | 354.64±343.8 | 60.15±41.8 |
| Abbreviations: CHr,reticulocyte Hemoglobin Content; TSAT, Transferrin Saturation | ||||||
Table 2 Results of the Functional Iron Parameters and Iron Status.
Serum iron values, serum transferrin, TSAT, ferritin, and hepcidin, they did not significantly changed over the study (Table 2A). In patients that not received iron prior the study we observed an increase in the serum iron levels and TSAT with a decrease in the serum ferritin levels and serum hepcidin (Table 2B). These findings, which not reached a significant difference, were not observed in patients that before the study received a 100 mg of iron a week as a maintenance therapy (Table 2C).
Inflammation influence
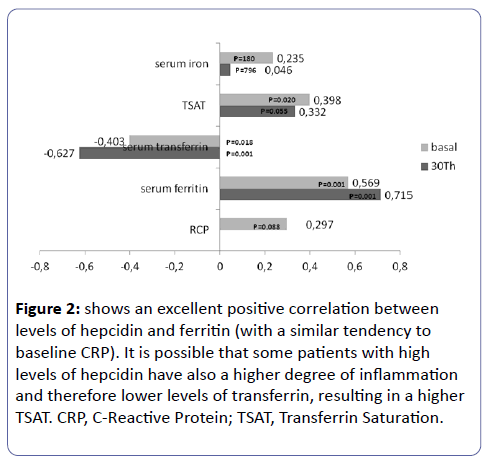
There was not a positive correlation between the CRP levels, EA parameters and FI: CHr (Figure 2), serum iron (r= -0.144; p=0,394) or TSAT (r= -0.049; p=0.772).
Figure 2: shows an excellent positive correlation between levels of hepcidin and ferritin (with a similar tendency to baseline CRP). It is possible that some patients with high levels of hepcidin have also a higher degree of inflammation and therefore lower levels of transferrin, resulting in a higher TSAT. CRP, C-Reactive Protein; TSAT, Transferrin Saturation.
Safety and tolerability
The tolerance of direct iron sucrose administration was good. No serious adverse events were observed beyond the study.
Discussion
The direct administration in the venous line of a little quantity of iron at the end of every HD session does not produce significant changes in the EA; evaluated by the reticulocytes count in peripheral blood. The majority of HD studies use as an activity markers the final products of the erythropoiesis (Hb or Htc); however, these parameters need a 60 days minimum observation period [13], the necessary time to replace previously existing erythrocyte for another one generated by the new erythropoietic therapy. We decide to use the reticulocyte parameter because of his short half-life (near 24 hours) [14] and for his rapid presence in the peripheral circulation, allowing his determination at 15 days inclusive [15]. This fact allowed shortening the period of study that allowed minimize the intercurrent processes as: infections, bleeding, or neocytolysis, preventing the outflow of patients from the study. Other EA markers as the eritron transferrin uptake [16] or the soluble transferrin receptor [15] also reduce the observation period; however, its determination is more complex and more expensive.
Another primary objective was to evaluate the FI with this therapy.
FID is a state in which there is insufficient iron incorporation into erythroid precursors in the face of apparently adequate body iron stores, as defined by the presence of stainable iron in the bone marrow together with a serum ferritin value within normal limits [17]. Recently, have been published some guides for diagnosis [17], because the classic parameters do not shows the sensitivity and specificity required [18,19]. The best indicator of FID are the percentage of hypochromic red cells (% HRC) which reflects the long-term deficits and the reticulocyte haemoglobin content (CHr) which, reflects the recent availability of iron for Hb synthesis [19]. CHr > 29 pg is indicative of an adequate iron incorporation into the developing erythron. However, some patients with these levels respond to IV intravenous iron therapy leading to a suggested cut-off value of 32 pg [17]. In our study the administration of a little iron bolus dose in every HD session do not change the FI, staying almost invariably in the three measured periods.
Despite of these findings, we thought that the IV iron maintenance therapy used in the present study could be indicated in base to following considerations. First, when we introduce IV iron in a short time, we can avoid a possible denaturation that can happen when iron in saline solutions stays for long time periods. Besides, when iron is administered once patients finish HD session prevents any possible dialytic lost. Second, these patients have inflammation more frequently, clinical condition that produced an iron store and availability reduction once administered. [17]. Therefore, the use in these cases of large, single iron doses, socalled load and hold, can increase the multi-organ iron deposits and don't cover the daily medullary necessity. On the contrary, a dispensation several times a week can increase the iron presence in the bloodstream and the availability in bone marrow. Third, in inflammatory and/or malnutrition states the transferrin levels decrease, and with it, his capacity of the catchment and transport after iron administration. Use of low doses of iron makes easier both, the capacity and the transport, avoiding the formation of significant amounts of nontranferrin bound iron (NTBI), also called “free iron”, a form of iron that might induce oxidative stress and cellular damage [20].
Another important aspect in the iron therapy is the doses that those patients need to balance the annual iron losses. The dose prescribed has been increased in most countries over the past 10-15 years [1,11]; however, benefits from IV iron must be balanced against potential risks. Recently Bailie et al reports an 18% increased risk of all-cause mortality with a 4-month dose of ≥400 mg/month compared with 100-299 mg/month doses [21]. Similarly Miskulin et al found a trend of increases risk of infection related mortality when cumulative iron doses exceeded 1050 mg over 3 months or 2100 over 6 months [22]. Others authors report similar results [23]. We used a dose that can be considered safety (240 mg/month) and besides, we observed that those patients that previously received a maintenance doses superior (400 mg/ month), now with this pattern they maintain either an EA and FI levels, decreasing the excessive iron exposition and the possible risk of mortality, hospitalization or both.
The hepcidin has emerged like the main iron regulatory. It is present in all cells involved in iron homeostasis. This 25-amino acid peptide act degrading ferroportin, the only known iron export, decreases iron absorption from the gastrointestinal tract and decreases the accessibility of stored iron from macrophages and the hepatocytes [24]. Its synthesis is up regulated in the liver by the iron status (via transferrin receptor: TfR1 and TfR2), and the setting of chronic inflammation stimulated by cytokines (which interleukin 6 is the most important) and is cleared by kidneys, so its levels rise according advances the renal disease[25]. In our study, we find high hepcidin levels similar to reports by other authors in HD patients [26,27]; observing also an excellent correlation between the ferritin and hepcidin, and a tendency between the hepcidin and RCP levels (Figure 1), both findings are expected because the hepcidin and ferritin share the same mechanism regulations [25]. Nowadays, the IV iron administration is a reason for concern, because unlike oral route the IV route escapes of the hepcidin regulation; and besides, for to be a repeatedly therapy would further increase blood hepcidin levels and thereby increase the subsequent iron blockade [28]. Consistent with continued dysregulation, a high iron concentration was found in the liver of HD patients who received IV iron therapy [18]. Otherwise, recently it has been shown that hepcidin-25 levels were associated with fatal and nonfatal cardiovascular events, even after adjustment for inflammation, what could be explained by the excessive iron deposition in the macrophages, which enhances oxidative stress in atherosclerotic plaques [29]. Therefore, that is interesting to us, to see the behaviour of the hepcidin levels in the 13 patients that previously to the study hadn’t received iron maintenance therapy. In then, after the administration of this pattern the FI parameters are increased slightly but avoid the increase of hepcidin levels (just like the ferritin).
Our study presents some limitations: is observational and not controlled; besides, has a small sample. Another possible confusion effect is that not all of patients had received IV iron maintenance at the same doses before the study. Prospective studies are necessary, with bigger samples and same basal conditions, that can be measure the efficiency of this pattern and it possible effect in the tissular deposits and in the NTBI.
Acknowledgements
The authors acknowledge to Amgen the adequate Kit for the hepcidin determination.
References
- Charytan DM, Pai AB, Chan CT, Coyne DW, Hung AM, et al. (2015) Considerations and challenges in defining optimal iron utilization in hemodialysis. J Am SocNephrol 26: 1238-1247.
- Besarab A, Bolton WK, Browne JK, Egrie JC, Nissenson AR, et al. (1998) The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med 339: 584-590.
- Drüeke TB, Locatelli F, Clyne N, Eckardt KU, Macdougall IC, et al. (2006) Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med 355: 2071-2084.
- Singh AK, Szczech L, Tang KL, Barnhart H, Sapp S, et al. (2006) Correction of anemia with epoetinalfa in chronic kidney disease. N Engl J Med 355: 2085-2098.
- Wetmore JB, Peng Y, Monda KL et al. (2015) Trends in Anemia Management Practices in Patients Receiving Haemodialysis and Peritoneal Dialysis: A Retrospective Cohort Analysis. Am J Nephrol 41: 354-361
- Rhee CM, Kalantar-Zadeh K (2013) Is iron maintenance therapy better than load and hold? J Am SocNephrol 24: 1028-1031.
- Freburger JK, Ellis AR, Kshirsagar AV, Wang L, Brookhart MA (2014) Comparative short-term safety of bolus versus maintenance iron dosing in hemodialysis patients: a replication study. BMC Nephrol 15: 154.
- Drüeke TB, Parfrey PS (2012) Summary of the KDIGO guideline on anemia and comment: reading between the (guide)line(s). Kidney Int 82: 952-960.
- Locatelli F, Bárány P, CovicA et al. Kidney Disease: Improving Global Outcomes guidelines on anaemia management in chronic kidney disease: a European Renal Best Practice position statement.
- Susantitaphong P, Alqahtani F, Jaber BL (2014) Efficacy and safety of intravenous iron therapy for functional iron deficiency anemia in hemodialysis patients: a meta-analysis. Am J Nephrol 39: 130-141.
- Bailie GR, Larkina M, Goodkin DA, Li Y, Pisoni RL, et al. (2013) Variation in intravenous iron use internationally and over time: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant 28: 2570-2579.
- https://www.viforpharma.es/wAssetsViforES/bin/es/Products/Ficha-tecnica-Venofer.pdf
- Vos FE, Schollum JB, Coulter CV, Doyle TC, Duffull SB, et al. (2011) Red blood cell survival in long-term dialysis patients. Am J Kidney Dis 58: 591-598.
- Krzyzanski W, Brier ME, Creed TM, Gaweda AE (2013) Reticulocyte-based estimation of red blood cell lifespan. ExpHematol 41: 817-822.
- Lorenzo JD, Rodríguez MM, Martín SS, Romo JM (2001) Assessment of erythropoiesis activity during haemodialysis therapy by soluble transferrin receptor levels and ferrokinetic measurements. Am J Kidney Dis 37: 550-556
- Cazzola M, Pootrakul P, Huebers HA, Eng M, Eschbach J, et al. (1987) Erythroid marrow function in anemic patients. Blood 69: 296-301.
- Thomas DW, Hinchliffe RF, Briggs C, Macdougall IC, Littlewood T, et al. (2013) Guideline for the laboratory diagnosis of functional iron deficiency. Br J Haematol 161: 639-648.
- Ferrari P, Kulkarni H, Dheda S, Betti S, Harrison C, et al. (2011) Serum iron markers are inadequate for guiding iron repletion in chronic kidney disease. Clin J Am SocNephrol 6: 77-83.
- Besarab A, Szczech L (2014) Uses and interpretation of iron studies in patients on chronic dialysis. Semin Dial 27: 579-581.
- Macdougall IC, Geisser P (2013) Use of intravenous iron supplementation in chronic kidney disease: an update. Iran J Kidney Dis 7: 9-22.
- Bailie GR, Larkina M, Goodkin DA, Li Y, Pisoni RL, et al. (2015) Data from the Dialysis Outcomes and Practice Patterns Study validate an association between high intravenous iron doses and mortality. Kidney Int 87: 162-168.
- Miskulin DC, Tangri N, Bandeen-Roche K, Zhou J, McDermott A, et al. (2014) Intravenous iron exposure and mortality in patients on hemodialysis. Clin J Am SocNephrol 9: 1930-1939.
- Fishbane S, Mathew AT, Wanchoo R (2014) Intravenous iron exposure and outcomes in patients on hemodialysis. Clin J Am SocNephrol 9: 1837-1839.
- Ganz T (2003) Hepcidin, a key regulator of iron metabolism and mediator of anemia of inflammation. Blood 102: 783-788.
- Tsuchiya K, Nitta K (2013) Hepcidin is a potential regulator of iron status in chronic kidney disease. TherApher Dial 17: 1-8.
- Zaritsky J, Young B, Wang HJ, Westerman M, Olbina G, et al. (2009) Hepcidin--a potential novel biomarker for iron status in chronic kidney disease. Clin J Am SocNephrol 4: 1051-1056.
- Ashby DR, Gale DP, Busbridge M, Murphy KG, Duncan ND, et al. (2009) Plasma hepcidin levels are elevated but responsive to erythropoietin therapy in renal disease. Kidney Int 75: 976-981.
- Gaweda AE, Ginzburg YZ, Chait Y, Germain MJ, Aronoff GR, et al. (2015) Iron dosing in kidney disease: inconsistency of evidence and clinical practice. Nephrol Dial Transplant 30: 187-196.
- van der Weerd NC, Grooteman MP, Bots ML et al,(2013) and CONTRAST Investigators. Hepcidin-25 is related to cardiovascular events in chronic haemodialysis patients. Nephrol Dial Transplant 28: 3062-3071
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences