The Effects of Aquatic Exercise on Functional Capacity and Health-Related Quality of Life in Hemodialysis Patients
Samara Anastasia, Kouidi Evangelia, Fountoulakis Konstantinos, Alexiou Serafeim, Deligiannis Asterios
DOI10.21767/2472-5056.100015
Samara Anastasia1*, Kouidi Evangelia1, Fountoulakis Konstantinos2, Alexiou Serafeim1 and Deligiannis Asterios1
1Laboratory of Sports Medicine, Department of Physical Education and Sport Sciences, Aristotle University of Thessaloniki, Thessaloniki, Greece
2Department of Medicine, Aristotle University of Thessaloniki, Thessaloniki, Greece
- *Corresponding Author:
- Samara Anastasia
Laboratory of Sports Medicine
Department of Physical Education and Sport Sciences
Aristotle University of Thessaloniki
Thessaloniki, Greece
Tel: 00306947454790
E-mail: samaranatasa@gmail.com
Received Date: June 16, 2016; Accepted Date: July 15, 2016; Published Date: July 18, 2016
Citation: Anastasia S, Evangelia K, Konstantinos F, Serafeim A, Asterios D (2016) The Effects of Aquatic Exercise on Functional Capacity and Health-related Quality of Life in Hemodialysis Patients. J Clin Exp Nephrol 1:15. doi: 10.21767/2472-5056.100015
Copyright: © 2016 Anastasia S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: The aim of this study was to evaluate the effect of an aquatic program in functional capacity and quality of life in hemodialysis patients.
Patients and methods: The study included 27 patients. Group A (n=15) followed an exercise program in a swimming pool and group B (n=12) were the controls. Six Minute Walk tests, Sit to Stand test, Sit and Reach test, Handgrip test, Timed Up and Go test were evaluated. All participants also completed SF-36 Questionnaire.
Results: After the aquatic program improvement was observed in all physical parameters and quality of life questionnaire in exercise group. The 6MWT distance increased from 558.8 ± 127.5 m to 625.6 ± 128.1 (p<0.05), the Sit to Stand test from 17.6 ± 5.2 sec to 15.2 ± 5.4 (p<0.05), Handgrip strength test from 34.6 ± 14.2 kg to 37.2 ± 14.7 (p<0.05), Sit and Reach test from 4.7 ± 9.1 cm to -0.6 ± 8.4 (p<0.05), Timed Up and Go test from 5.5 ± 1.4 sec to 4.6 ± 1.4 (p<0.05). Group B reduced its performance in 6-Min walk test from 499.1 ± 94.6 m to 454.4 ± 90.4 (p<0.05), Handgrip test from 34.3 ± 9.6 kg to 32.3 ± 9.9 (p<0.05), and Timed Up and Go from 6.1 ± 1.7 sec to 6.6 ± 2.5 (p<0.05). In SF-36 questionnaire, Group A improved both in Physical and Mental Component Scale and compared to Group B.
Conclusion: The results demonstrated that aquatic exercise improves physical functioning and quality of life in hemodialysis patients.
Keywords
Aquatic exercise; Chronic kidney disease patients; Functional capacity; Quality of life
Introduction
Chronic kidney disease patients on hemodialysis (HD) show significantly diminished exercise capacity, tolerance, strength and endurance, compared to healthy individuals. Anaemia, cardiac dysfunction, muscle abnormalities, depression and sedentary lifestyle affect negatively their functional capacity, as well as their reported quality of life [1,2]. Low levels of physical activity levels in HD patients have been associated with increased risk of hospitalization and rates of morbidity [3].
It is well established by studies that exercise rehabilitation programs contribute positively to an improvement in the functional capacity and psychosocial status of HD patients [4-6]. Aerobic and resistance exercise programs have been applied to patients during HD or in rehabilitation centers [1,5], with numerous beneficial effects, although outpatient exercise training has been proved to be more effective compared to intradialytic exercise [1]. Despite the established benefits of exercise training programs, dropout rate remains high due to lack of motivation [7]. Thus it is required the implementation of alternative forms of exercise in order to increase patients’ participation and compliance.
In recent studies, aquatic rehabilitation programs have been proven to improve physical capacity in a wide range of diseases, such as chronic heart failure, coronary artery disease, chronic obstructive pulmonary disease, osteoarthritis and multiple sclerosis [8-11].
Aquatic exercise through water’s physical properties, such as buoyancy, hydrostatic pressure, viscosity and density, provides an ideal environment to exercise throughout the year. The buoyancy of water supports body weight resulting in reduced joint loading and improved flexibility. The resistive forces of viscous drag and turbulence provide resistance to movements, which helps muscle strengthening. Exercises in water can also improve agility, balance, and cardiovascular fitness and minimizes the risk of falls when compared to exercise on land [11,12].
Although there is growing interest of innovative forms of exercise on renal function in patients with moderate renal failure, there is no study to date concerning aquatic exercise on HD patients. Therefore, the purpose of this study was to evaluate the effectiveness of an aquatic exercise program on functional capacity and health related quality of life in chronic kidney disease patients on hemodialysis.
Patients and Methods
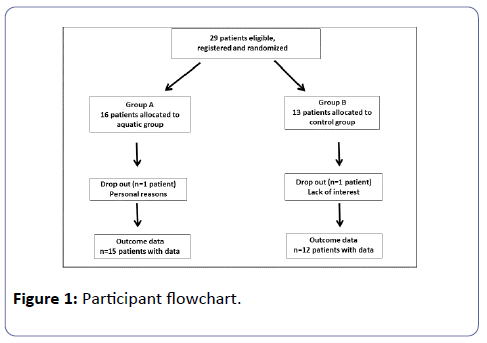
Twenty nine patients, male (n=24) and female (n=5), with chronic kidney disease on hemodialysis, volunteered to participate in the study from a total of 200 patients from major nephrology clinics of Thessaloniki after a short briefing of the research. They were randomly assigned by simple allocation (drawing lots) to either a 4-month therapeutic aquatic exercise program (Group A-15 patients), or control status (Group B- 12 patients). Inclusion criteria were primarily to be evaluated by the participant’s nephrologist who gave authorization to exercise testing. All patients should also be on hemodialysis three days per week, 4 hours/session, for at least six months prior to the study and there should be no acute or chronic medical conditions that would affect the measured data. Exclusion criteria were recent myocardial infarction (within 6 weeks), malignant arrhythmias, or unstable angina. Hemoglobin level should be above 10 gr/dl and constant throughout the study, and medical prescription should not involve b-blockers or other anti-arrhythmic medication. In Group a fifteen subjects (thirteen male) completed all phases of assessment and intervention. In Group B twelve subjects (eleven male) were also assessed, at the beginning and at the end of four months. Two patients dropped out of the study due to lack of interest and for personal reasons (family health issues). The participants had to be in a clinically stable condition for at least three months before entering the study and remained in a stable medication regimen during the study. They were also asked to refrain from any other form of recreational activity during the study period and required to fulfil the 80% attendance during the training programs. In addition, Group B had no formal intervention and was asked to continue their usual sedentary lifestyle. All patients were informed about the purpose and the procedures of the study and gave written informed consent, according to the Ethical Committee of the Aristotle University.
Study Design
Physical fitness assessment-exercise testing
The physical capacity of all patients at the beginning of the study was determined on an “off” dialysis day with the following functional capacity tests.
1. Six Minute Walk Test (6MWT), an indirect test to estimate cardiovascular endurance and functional capacity (13-14). The participants were asked to walk the longest distance possible in 6 minutes by walking continuously (not running or jogging) on a 20 meter measured corridor, turning around at the final mark without stopping and covering as much as ground possible. They could stop if needed and restart. The distance covered in meters was recorded at the end of the test. The 6MWT is one of the most utilized tests in chronic diseases [13,14]. It is easy to apply, almost costless, quick in performing, and is considered to be a better indicator of the ability to perform activities that resemble those of daily living, such as walking, than physiological exercise capacity testing [15].
2. Sit to Stand test, to specify muscular strength, measured the time (in seconds) required to perform 10 consecutive repetitions of sitting down and getting up from a chair. Participants were instructed to perform the task “as fast as possible”, starting and finishing at the sitting position. They began the test by crossing their arms on the chest and sitting with their backs against the chair [16]. This test is simple, inexpensive, rapid and reproducible and is used for people with renal disease [15,17,18].
3. Sit and Reach test was used to measure flexibility of hamstrings and lower back [19]. Patients were sat with their legs spread ahead, their heels touching the specific instrument and their palms one on top of the other. They should bend their torso over, keeping the position for two seconds without bending the knees. The best of three trials was recorded, in centimetres, as the distance of the middle finger till the measurement instrument on the box.
4. A handgrip dynamometer (Baseline Handgrip Dynamometer) was used to measure the power of dominant upper arm. Participants were in the sitting position, holding the dynamometer so that the forearm was at a right angle with the upper arm with the elbow close to the body. Three consecutive maximal repetitions of 3 seconds each, with 10 seconds of rest between the repetitions, were performed with the dominant arm. The average measurement in kg was recorded [15].
5. Finally, Timed Up and Go test was used to evaluate functional mobility [20]. Patients rose from a standard, armless chair to a full standing position, walked 3 m, turned around and returned to the seated position, performing these manoeuvres as fast as possible. Walking speed was determined to the nearest 0.01s.
Health-related quality of life assessment
All patients were also requested to complete the Short Form-36 Questionnaire (SF-36), in the first week of admission and at the end of the study. It is a multipurpose, short-form health survey with 36 questions, which yielded an 8-scale profile of scores as well as Physical Component Scale and Mental Component Scale summary measures. It was translated and standardized for the Greek Population [21].
Aquatic exercise program
Aquatic training was conducted in water on non-dialysis days, for a period of 4 months, three times a week for 60 minutes at a time. Patients were required to attend at least 80% of all sessions over the four-month period. At the start the intensity of the program was based on individual’s tolerance and further gradually modified by the patients’ perceived exertion and adaptation to the training program. Thus, exercise intensity and prescription was gradually increased as physiological adaptations occurred. During the training sessions heart rate was measured in each interval between the activities. Patients also rated their perceived exertion on a Borg Scale. They were encouraged to reach perceived exertion 13–14 (somewhat hard) on the Borg 6–20 category scale. The aquatic exercise program was constructed and supervised by an experienced exercise trainer, specialized in chronic diseases rehabilitation programs. The warm-up period lasted 10 minutes and included stretching exercises. Then the patients entered the pool and swam, gradually from 20 minutes at the beginning of the program to 40 minutes, according to individuals’ tolerance, with various types of swimming (free style, breast stroke, and back stroke) using foam tubes, buoyancy belts, and paddles. Relaxation exercises were conducted for 10 minutes after every session, including stretching and breathing exercise techniques.
Statistical analysis
All statistical analysis was performed using the Statistical Package for Social Sciences (SPSS Inc, Chicago, IL), version 16.0, software for Windows (Microsoft Corp, Redmond, WA). The Kolmogorov–Smirnov test was used to examine the normality of the distribution. Changes of variables within the groups at baseline and the end of the study were evaluated by two-way ANOVA with repeated measures of variance with time and group being the independent variables. In addition, within group change from baseline was obtained by subtracting the final from the baseline values. Data are expressed as mean SD, with a significance level p<0.05.
Results
A total of 93.1% of participants (27 patients) completed all exercise sessions (Figure 1). The demographic and clinical characteristics of the 27 patients are shown in Table 1. The results obtained from the functional capacity assessments, at baseline and follow-up, are presented in Table 2. All the exercised patients at the end of the study showed significant improvements in their health-related quality of life results (Table 3). In specific, after 4 months of training, the patients who attended the aquatic exercise program showed a significant improvement in the distance measured in 6-MWT by 12%, compared to initial assessment, walking 67 meters more (p<0.05). Furthermore, group A improved by 28.69% (p<0.05), compared to group B. Finally, group B showed a reduction of functional capacity by 9.74% (p<0.05) compared to its initial 6MWT assessment. In Sit to Stand test, group A improved initial measurement by 13.63% (p<0.05), being able to finish the test in 2.4 seconds quicker and thus group A improved in comparison to group B by 39.47% (p<0.05) showing a tendency. In Handgrip test, group A increased by 7.51% (p<0.05) the initial assessment, and group B showed a statistically significant decline by 5.84% (p<0.05), but even so, no statistical differences among groups were observed. In Sit and Reach test, group A improved first measurement by 87.24% (p<0.05) and also compared to group B follow up (p<0.05). Group B also diminished its initial assessment (p<0.0). In Timed Up and Go test, group A improved its initial assessment by 16.36% (p<0.05) and increased the difference by almost 50% compared to group B (p<0.05).
| Group Α (n=15) |
Group B (n=12) |
P value | |
|---|---|---|---|
| Male/Female | 13/2 | 11/1 | |
| Age (years) | 48.0±11.3 | 48.6±15.4 | 0.4 |
| BMI (kg/m2) | 24.23±2.81 | 25.46±5.14 | 0.9 |
| Ht(%) | 36.8±3.4 | 36.3±3.7 | 0.7 |
Table 1: Demographic and clinical characteristics of the patients who completed the study (mean ± SD). Group Α=patients who followed aquatic training program, Group Β=Control Group; BMI: Body Mass Index; Ht: Hematocrit.
| Group A | Group B | Group A vs Group B | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow up |
P value | Baseline | Follow up |
P value | Baseline | Follow up |
|
| 6min walk test (m) |
558.8±127.5 | 625.6±128.1 | .000 | 499.1±94.6 | 454.4±90.4 | .002 | .189 | .001 |
| Sit to stand (sec) | 17.6±5.2 | 15.2±5.4 | .000 | 20.2±6.7 | 21.2±6.5 | .381 | .270 | .032 |
| Handgrip (kg) | 34.6±14.2 | 37.2±14.7 | .002 | 34.3±9.6 | 32.3±9.9 | .025 | .956 | .337 |
| Sit and reach (cm) | 4.7±9.1 | -0.6±8.4 | .000 | 8.1±12.1 | 11.3±12.7 | .049 | .408 | .010 |
| Timed up and go (sec) | 5.5±1.4 | 4.6±1.4 | .002 | 6.1±1.7 | 6.6±2.5 | .090 | .313 | 0.14 |
Table 2: Results of field tests of the groups at the beginning and the end of the training program (Mean ± SD). Group Α=patients who followed aquatic training program, Group Β=control group.
| Group A | Group B | Group A vs Group B | ||||||
|---|---|---|---|---|---|---|---|---|
| SF-36 | Baseline | Follow up | P value | Baseline | Follow up | P value | Baseline | Follow up |
| PCS | 45.5±6.6 | 49.9±6.6 | .001 | 46.3±8.1 | 43.9±8.8 | .063 | .795 | .054 |
| MCS | 44.5±10.7 | 53.3±6.9 | .000 | 41.9±10.2 | 39.0±10.4 | .192 | .521 | .000 |
Table 3: Scores of quality of health- related quality of life indices. Values are mean ± SD. PCS: Physical Component Scale; MCS: Mental Component Scale.
Quality of life results
After the training program, in regards of the Physical Component Scale, group A showed statistically significant improvement by 9.67% (p<0.05). On the contrary, group B showed a decrease by 5.19%, but not statistically significant.
In Mental Component Scale group Α showed improvement after 4 months by 19.77% (p<0.05) and 26.83% (p<0.05) compared to follow ups with group B.
Discussion
The results of the present study demonstrated that an aquatic exercise program has favourable effects on functional capacity in patients with chronic kidney disease on hemodialysis, indicating that exercise in water can be used as an alternative mode of exercise training in these patients. Even more, aquatic training helps improve health related quality of life, with its two branches, physical and mental aspect.
Previous research has shown significant benefits from exercise rehabilitation programs in health centers in HD patients. To date, there is shortage of evidence from randomized controlled studies on the effectiveness of aquatic exercise in chronic kidney disease patients on hemodialysis.
The performance at submaximal test (6MWT) improved by almost 67 meters, as aquatic exercise has been proposed as an effective form of exercise for improving overall fitness especially in individuals with low levels of physical fitness [22]. Relative improvements have been found in previous studies in respect to oxygen consumption and duration of exercise [5,15]. Increase of oxygen consumption is reported to be 20-40% in exercise programs on non-dialysis days in organized health centers, probably due to longer exercise duration or exercise intensity [5,23-25]. In a study from Moore et al. [26], of short duration (three months) and low impact aerobic exercise, patients physical fitness improved by 13% in accordance to this study.
Sit to Stand test is used as an indirect measurement of lower extremities strength, but can also reflect various parameters as balance, cardiovascular endurance, coordination, flexibility and satisfying range of motion [27]. In the present study HD patients improved their performance by almost 2.4 seconds, a corresponding finding to previous studies [18]. The improvement is statistically significant even though it is reported that high functional patients lack in comparison to healthy individuals [28]. The various properties of water, such as buoyancy, hydrostatic pressure and viscosity offer a unique advantage of safe training in health maintenance in chronic diseases [12]. This applies to AV fistula as well, since nephrologist’s advice that once the surgical site has healed, there are no restrictions on swimming or showering [29].
Uremic myopathy leads to loss of muscle mass and power. Regarding maximum strength of upper extremities Chang et al. [29] have recorded to be an independent factor of renal disease progression, as well as that grip strength is reduced in opposition to age. The present study showed that aquatic training in HD patients increased strengthening upper extremities muscles by 7.51%. This is consistent to other studies in which patients benefit from resistance exercise programs not only to preserve but to improve their muscular strength [18]. The resistive effect of water provides exercise loading during movement, which enhances muscular tension and increases energy expenditure beyond that achieved with land exercises [30].
The Sit to stand manoeuvre is another key functional activity of daily life. Flexibility of hamstrings in this study has shown significant improvement in aquatic exercising patients while controls showed a reduction of muscle elasticity. These findings are consistent with previous studies of Jang & Kim [31], in an exercise program of 12 weeks during hemodialysis and of Ling et al. [32] in a 3-month home exercise program of Tai Chi.
A usual test of neuromuscular function in chronic diseases is Timed Up and Go. Improvements through exercise have been reported in prior studies [19,32-34], consistent to the present study. In specific Heiwe et al. [33] with an exercise program of 12 weeks improved muscular function and walking ability of elderly patients with renal disease. Bullani et al. [35] reported significant improvement in Timed Up and Go test after a resistance training program (with Thera bands) during hemodialysis. The reduction in time required to complete the test is possibly attributed to the increase in muscle strength of lower extremities due to exercise in water. Moreover, these findings comply with previous researches reporting that it is highly important for HD patients the strengthening of lower extremities because it is combined with increased stability, sense of improved physical fitness and more effective handling of everyday activities [32].
Studies that have been conducted in other chronic diseases in regards to the effect of aquatic exercise programs, have shown that the advantages of training in the water are equal or even better than training in the land, such as walking or running. In specific a research conducted in a data base with more than 30.000 people in Cooper Clinic, has proved that the overall health benefits from training in water are comparable to training in land, with addicted advantage the wider range of application in special populations [36,37]. Finally, aquatic exercise has been reported to have beneficial effects in aerobic capacity and muscle strength in coronary artery disease patients, compared to land exercise [11].
Previous studies have strongly suggested that patients with chronic kidney disease on hemodialysis are traditionally described as suffering from reduced health-related quality of life owing to general fatigue, exertional dyspnea during everyday activities, frequent hospitalizations, frustration, anxiety and depression [1,4,6].Thus regarding the evaluation of the effect of an aquatic exercise program to the quality of life of hemodialysis patients, a significant improvement was reported to the exercise group compared to control group. Similar finding have been ascertained in prior studies [4,25,38,39]. It is important to be noted that in exercising patients both parameters of SF-36 questionnaire were improved, physical and mental, while in controls there has been deterioration. Studies that have been conducted in other chronic diseases such as multiple sclerosis and osteoarthritis are in accordance the present study, reporting that aquatic exercise improves patients’ health-related quality of life [8,40]. Among the psychological benefits of aquatic exercise are improved confidence, a more positive attitude (individually and as a group), a feeling of well-being, less stress and tension and more social interaction [41].
Results of this study must be interpreted in the face of certain method limitations. Outcomes including the clinical importance were not assessed. Also, a potential limitation is that patients living far away from a swimming pool don’t have the possibility to attend an aquatic program. Furthermore it became evident even during the initial briefing of patients, a reluctance of female patients to participate in sports activities. Lack of free time and social reasons were usually the justification. Finally, middle age patients volunteered to participate and not elderly ones, probably due to greater familiarity to water sport activities. Apart to these limitations the results of the present study demonstrate that an aquatic exercise program improves functional capacity, cardiorespiratory fitness and quality of life in patients with chronic kidney disease on hemodialysis. Thus, aquatic exercise may be used as an alternative mode of exercise in rehabilitation programs aiming to increase exercise adherence in patients with chronic kidney disease on hemodialysis.
On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
- Kouidi E, Grekas D, Deligiannis A, Tourkantonis A (2004) Outcomes of long-term exercise training in dialysis patients: comparison of two training programs. ClinNephrol 61 Suppl 1: S31-38.
- Deligiannis A, Kouidi E, Tourkantonis A (1999) Effects of physical training on heart rate variability in patients on hemodialysis. Am J Cardiol 84: 197-202.
- Sietsema KE, Amato A, Adler SG (2004) Exercise capacity as a predictor of survival among ambulatory patients with end-stage renal disease. Kidney Int 65: 719-724.
- Ouzouni S, Kouidi E, Sioulis A, Grekas D, Deligiannis A (2009) Effects of intradialytic exercise training on health-related quality of life indices in haemodialysis patients. ClinRehabil 23: 53-63.
- Konstantinidou E, Koukouvou G, Kouidi E, Deligiannis A, Tourkantonis A (2002) Exercise training in patients with end-stage renal disease on hemodialysis: comparison of three rehabilitation programs. J Rehabil Med 34: 40-45.
- Kouidi EJ (2001) Central and peripheral adaptations to physical training in patients with end-stage renal disease. Sports Med 31:651-65.
- Painter P, Carlson L, Carey S, Myll J, Paul S (2004) Determinants of exercise encouragement practices in hemodialysis staff. NephrolNurs J 31:67-74.
- Jigami H, Sato D, Tsubaki A, Tokunaga Y, Ishikawa T, et al. (2012) Effects of weekly and fortnightly therapeutic exercise on physical function and health-related quality of life in individuals with hip osteoarthritis. J OrthopSci 17: 737-44.
- Rae S, White P (2009) Swimming pool-based exercise as pulmonary rehabilitation for COPD patients in primary care: feasibility and acceptability. Prim Care Respir J 18: 90-94.
- Teffaha D, Mourot L, Vernochet P, Ounissi F, Regnard J, et al. (2011) Relevance of water gymnastics in rehabilitation programs in patients with chronic heart failure or coronary artery disease with normal left ventricular function. J Card Fail 17: 676-683.
- Volaklis KA, Spassis AT, Tokmakidis SP (2007) Land versus water exercise in patients with coronary artery disease: effects on body composition, blood lipids, and physical fitness. Am Heart J 154:560-566.
- Becker BE (2009) Aquatic therapy: scientific foundations and clinical rehabilitation applications. PM R 1: 859-872.
- Fitts SS, Guthrie MR (1995) Six-minute walk by people with chronic renal failure. Assessment of effort by perceived exertion. Am J Phys Med Rehabil 74:54-58.
- Solway S, Brooks D, Lacasse Y, Thomas S (2001) A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest. 119:256-270.
- Depaul V, Moreland J, Eager T, Clase CM (2002) The effectiveness of aerobic and muscle strength training in patients receiving hemodialysis and EPO: a randomized controlled trial. Am J Kidney Dis 40:1219-1229.
- Parsons TL, Toffelmire EB, King-Van Vlack CE (2006) Exercise training during hemodialysis improves dialysis efficacy and physical performance. Arch Phys Med Rehabil 87:680-687.
- Csuka M, McCarty DJ (1985) Simple method for measurement of lower extremity muscle strength. Am J Med 78:77-81.
- Segura-Ortí E, Kouidi E, Lisón JF (2009) Effect of resistance exercise during hemodialysis on physical function and quality of life: randomized controlled trial. ClinNephrol 71:527-537.
- Macdonald J, Marcora S, Jibani M, Phanish M, Holly J, et al. (2005) Intradialytic exercise as anabolic therapy in hemodialysis patients- a pilot study. ClinPhysiolFunct Imaging 25:113-118.
- Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am GeriatrSoc 39:142-148.
- Anagnostopoulos F, Niakas D, Pappa E (2005) Construct validation of the Greek SF-36 Health Survey. Qual Life Res 14: 1959-1965.
- Sakai A, Oshige T, Zenke Y, Yoshiaki Y, Nagaishi H, et al (2010) Unipedal standing exercise and hip bone mineral density in postmenopausal women: a randomized controlled trial. J Bone Miner Metab 28:42-48.
- Cheema BS, Singh MA (2005) Exercise training in patients receiving maintenance hemodialysis: a systematic review of clinical trials. Am J Nephrol 25: 352-364.
- Deligiannis A, Kouidi E, Tassoulas E, Gigis P, Tourkantonis A, et al. (1999b) Cardiac response to physical training in hemodialysis patients: An echocardiographic study at rest and during exercise. Int J Cardiol 70:253-266.
- Kouidi E, Iacovides A, Iordanidis P, Vassiliou S, Deligiannis A, et al. (1997) Exercise renal rehabilitation program: psychosocial effects. Nephron 77:152-158.
- Moore GE, Parsons DB, Stray-Gundersen J, Painter PL, Brinker KR, et al. (1993) Uremic myopathy limits aerobic capacity in hemodialysis patients. Am J Kidney Dis 22: 277-287.
- Padilla J, Krasnoff J, Da Silva M, Hsu CY, Frassetto L, et al. (2008) Physical functioning in patients with chronic kidney disease. J Nephrol 21: 550-559.
- Blake C, O'Meara YM (2004) Subjective and objective physical limitations in high-functioning renal dialysis patients. Nephrol Dial Transplant 19: 3124-3129.
- Chang YT, Wu HL, Guo HR, Cheng YY, Tseng CC, et al. (2011) Handgrip strength is an independent predictor of renal outcomes in patients with chronic kidney diseases. Nephrol Dial Transplant 26: 3588-3595.
- Forrest KY, Zmuda JM, Cauley JA (2007) Patterns and correlates of muscle strength loss in older women. Gerontology 53: 140-147.
- Jang EJ, Kim HS (2009) Effects of exercise intervention on physical fitness and health-relalted quality of life in hemodialysis patients. J Korean AcadNurs 39: 584-593.
- Ling KW, Wong FS, Chan WK, Chan SY, Chan EP, et al. (2003) Effect of a home exercise program based on tai chi in patients with end-stage renal disease. Perit Dial Int 23 Suppl 2: S99-99S103.
- Heiwe S (2004) Experienced physical functioning and effects of resistance training in patients with chronic kidney disease [thesis]. Stockholm, Sweden: Karolinska Institute.
- Koh KP, Fassett RG, Sharman JE, Coombes JS, Williams AD (2010) Effect of intradialytic versus home-based aerobic exercise training on physical function and vascular parameters in hemodialysis patients: a randomized pilot study. American Journal of Kidney Diseases 55: 88-99.
- Bullani R, El-Housseini Y, Giordano F, Larcinese A, Ciutto L, et al. (2011) Effect of intradialytic resistance band exercise on physical function in patients on maintenance hemodialysis: a pilot study. J RenNutr 21:61-65.
- Chase NL, Sui X, Blair SN (2008) Comparison of the health aspects of swimming with other types of physical activity and sedentary lifestyle habits. Int J Aquatic Res Edu 2:151-161.
- Chase NL, Sui X, Blair SN (2008) Swimming and all-cause mortality risk compared with running, walking and sedentary habits in men. Int J Aquatic Res Educ 2:213-223.
- Yarlas AS, White MK, Yang M, Saris-Baglama RN, Bech PG, et al. (2011) Measuring the health status burden in hemodialysis patients using the SF-36® health survey. Qual Life Res 20:383-389.
- Samara AP, Kouidi E, Ouzouni S, Vasileiou S, Sioulis A, et al. (2013) Relationship between exercise test recovery indices and psychological and quality-of-life status in hemodialysis patients: a pilot study. J Nephrol 26: 495-501.
- Kargarfard M, Etemadifar M, Baker P, Mehrabi M, Hayatbakhsh R (2012) Effect of aquatic exercise training on fatigue and health-related quality of life in patients with multiple sclerosis. Arch Phys Med Rehabil 93: 1701-1708.
- The Kidney Foundation of Canada (2010) Some facts about the AV fistula.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences