Polymyxin B hemoperfusion improves hemodynamic status in patients with sepsis with both gram-negative and nongram- negative bacteria
Yoichiro Tanaka, Kazuhiro Okano, Ken Tsuchiya, Masakazu Yamamoto and Kosaku Nitta
DOI10.21767/2472-5056.100004
Yoichiro Tanaka1, Kazuhiro Okano1,2*, Ken Tsuchiya1,2, Masakazu Yamamoto3 and Kosaku Nitta1
1Department of Medicine, Kidney Center
2Department of Blood Purification, Kidney Center, and
3Department of Gastroenterology, Tokyo Women’s Medical University, Tokyo, Japan
- *Corresponding Author:
- Kazuhiro Okano
MD, 8-1 Kawadacho, Shinjukuku, Tokyo 162- 8666, Japan
Tel: +81-3-3353-8111
Fax: +81-3-5269-7368
E-mail: kaokano@kc.twmu.ac.jp
Received date: November 18, 2015 Accepted date: December 21, 2015 Published date: December 25, 2015
Citation: Tanaka Y, Okano K, Tsuchiya K, Yamamoto M, Nitta K (2015) Polymyxin B hemoperfusion improves hemodynamic status in patients with sepsis with both gram-negative and non-gram-negative bacteria. J Clin Exp Nephrol 1:4. DOI: 10.21767/2472-5056.100004
Copyright: © 2015 Tanaka Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Direct hemoperfusion with a polymyxin B (PMX) often produces improvement in patients with sepsis caused by bacteria other than those classified as gram-negative. The aim of the present study is to clarify the therapeutic effects of PMX in patients with sepsis caused by bacteria other than gram-negative bacteria.
Methods and Findings: We enrolled 41 patients with severe sepsis including various other diseases, which were treated with PMX. We evaluated the improvement in blood pressure, vasopressor requirement, respiratory condition, Sequential Organ Failure Assessment (SOFA), inotropic score, and serum biochemical markers before and after PMX therapy. PMX therapy improved inotropic scores (14.3 to 8.4, p?0.01) and small decrease partial SOFA scores (2.8 to 2.1, p?0.01). We compared hemodynamic scores between patients with gram-negative bacteria (GN group) and non-gram-negative bacteria (non-GN group). Changes in blood pressure, inotropic score and partial SOFA scores by PMX therapy showed no significant differences between the GN and non-GN groups (p = 0.26, p = 0.11 and
p = 0.3, respectively). Furthermore, we compared the 28-day mortality between GN and non-GN groups. As a result, there is no significant deference. (p = 0.85).
Conclusion: PMX therapy is effective to improve hemodynamic status of septic patients not only with gram-negative but with non-gram-negative bacteria. Main limitation is that the sample size was relatively small and the study was performed in a single center.
Key words
polymyxin B; endotoxin; non-gram-negative bacteria; inotropic score; SOFA score; 28-day mortality
Introduction
Direct hemoperfusion (DHP) with a polymyixin-B (PMX) column is used for patients with sepsis caused by gram-negative bacteria. This treatment is thought to be useful for removing endotoxins from the circulation: endotoxins mainly consist of lipopolysaccharides from the outer membrane component of gram-negative bacteria. PMX (Toray industries, Tokyo, Japan) has been commercially available in Japan since 1993. PMX therapy has been considered effective for patients with sepsis, particularly those with septic shock [1]. Although the column has been used worldwide, it remains unclear whether the therapy is significantly effective compared to other conventional treatments and what favorable effects it has on patients.
Conclusions about the effect of PMX therapy are controversial. Tani reported that the mean levels of plasma endotoxin were significantly reduced by PMX therapy [2]. There are reports mentioning that PMX therapy improved blood pressure (BP) and the ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen (the PaO2/FiO2 ratio) [3-4]. Cruz reviewed that the therapy appears to have favorable effects on mean arterial pressure (MAP), reduced dopamine use, improved the PaO2/ FiO2 ratio, and lowered patient mortality [5]. Further, there are a few randomized control trials (RCTs), suggesting the therapeutic benefits of this therapy. Patients treated with PMX demonstrated significant increases in cardiac index, left ventricular stroke work index, and oxygen delivery index compared with those without the treatment, whereas no significant improvements were observed between the groups in organ dysfunction as assessed by the Sequential Organ Failure Assessment (SOFA) [6]. Another report showed that there were significant differences between the two groups in MAP, the PaO2/FiO2 ratio, and vasopressor requirement, resulting in significant improvement of SOFA scores at 72 h after PMX therapy [7]. Inconsistent with these studies, a meta-analysis shows that there was no significant improvement in all-cause mortality at 28 days after the treatment [8]. However, there is a conflicting report that PMX therapy has beneficial effects on all-cause mortality [9]. In Japan, PMX therapy has been approved as one of treatment covered by the national insurance coverage, causing difficulty in performing RCTs. Using a retrospective cohort study design, we examined whether PMX therapy has some clinical benefits and whether PMX has therapeutic effects on sepsis caused by non-gram-negative bacteria. We believe our study extends some additional knowledge in this field
Methods
Patients
We enrolled 41 patients with sepsis receiving PMX therapy at our center between 2007 and 2012. We obtained the patient information from the electronic clinical records of the center. The data before 2006 could not be collected precisely because paper records were used before the introduction of electronic records. Therefore, we obtained all the PMX records, which have been performed in our center since 2007. The criteria of the American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference were used for the diagnosis of sepsis [10]. Most participants were suspected to have infection with gram-negative bacteria. In many cases, PMX was performed before the results of the bacterial culture because of participants’ serious conditions. Some patients had infection with grampositive or other bacteria, but we did not exclude these patients because PMX therapy was extensively performed and our aim was to examine the clinical effectiveness of PMX therapy for septic shock caused by any type of bacteria. Before starting the study, we obtained approval by the ethical committee of Tokyo Women’s Medical University. Patients or important members of family provided written given informed consent before entry of the present study.
PMX therapy
DHP was performed using a PMX-coated column, PMX 05-R (Toray, Tokyo, Japan). Each treatment was performed once for each patient with 2-3 h sessions and 50-100 mL/min of blood flow. In several patients, we performed the therapy for 2 consecutive days with the expectation of better prognosis. Nafamostat mesilate was used as the anti-coagulant, which has been used in patients with hemorrhagic conditions in Japan. Temporary catheter was used for vascular access in most patients except those with already present vascular access such as arterial-venous fistula.
Data collection and endpoint
Clinical histories and laboratory data were retrospectively collected from hospital records. Primary endpoints were BP, vasopressor requirement (based on inotropic and partial SOFA scores), the PaO2/ FiO2 ratio, conventional SOFA scores and serum biomarkers for systemic inflammation [C-reactive protein (CRP) and white blood cell (WBC)] and 28-day mortality. The inotropic score calculated as follows [11-12].
Inotropic score = (dopamine dose × 1) + (dobutamine dose × 100) + (noradrenaline dose × 100) + (phenylephrine dose × 100
Vasopressors agents are expressed in μg/kg/min. The inotropic score is useful for evaluating the total requirements of vasopressors and the effectiveness of the treatment among various patients [7].
The conventional SOFA score consists of six categories to evaluate multiple organ failure of septic patient [13]. Since cardiovascular category score is thought the most important factor to exacerbate severity of the SOFA score, we employed cardiovascular score of SOFA score alone, defined as partial SOFA score (pSOFA), which was used in the previous report [14-16]. We think that two different scores, pSOFA and inotropic score, could enable us to evaluate requirement of vasopressors more precisely. BP was measured hourly during PMX therapy using a mercury sphygmomanometer. Because, as observed from clinical records, serum endotoxin levels were not measured in any patients, we excluded these from one of the endpoints. We examined the laboratory data at baseline and at 72-h after PMX therapy. For patients who died within 72 h from the initiation of therapy, the last collectable data were used for evaluation.
Statistical analysis
Clinical parameters are expressed as mean ± standard deviation. Normally distributed variables were compared using the Student’s t-test and abnormally distributed variables using the Mann-Whitney U-test. Duration of survival was compared using log-rank test. A p-value of 0.05 was considered statistically significant. Data were analyzed with JMP version 11.
Results
The participants consisted of 32 males and 9 females (age range, 19-100 years) (Table. 1). Four patients were diagnosed with Escherichia coli infection. E. coli was the most common gram-negative bacteria detected from the bacterial cultures of peripheral blood samples but accounted for only 9.5% of the total bacteria. Microbiological analyses showed various bacterial infection in the patients, for whom bacterial cultures were obtained prior to or during PMX therapy. Gram-negative bacteria were detected in 13 patients (31.7%). Approximately half of the patients showed negative results for bacterial recovery, suggesting that PMX therapy was performed in patients without sepsis or that bacterial recovery was unsuccessful in some cases of sepsis. Another reason may be that PMX therapy was performed for many patients before obtaining the microbiological results because the conditions of the patients warranted immediate treatment. Norepinephrine/epinephrine and dopamine were used in 71% of the patients and dobutamine in 27% at the initiation of PMX therapy.
| n = 41 | |
|---|---|
| Male : Female (%) | 32 (78) : 9 (22) |
| Mean age (years old) (range) | 69.0 (19 – 100) |
| Bacteriology (%) | |
| Escherichia coli | 4 (9.5) |
| Bactrroidesfragilis | 2 (4.8) |
| Acinetobactorbaumannii | 2 (4.8) |
| Serratiamarcescens | 1 (2.3) |
| Klebsiellapneumonae | 1 (2.3) |
| Enterobactoraerogenes | 1 (2.3) |
| Streptococcus agalactiae | 1 (2.3) |
| Neisseria meningitides | 1 (2.3) |
| Enterococcus faecalis | 1 (2.3) |
| None | 20 (47.6) |
| Unknown | 6 (14.3) |
| Use of vasopressor (%) | |
| Norepinephrine / epinephrine | 30 (71) |
| Dopamine | 30 (71) |
| Dobutamine | 11 (27) |
| Baseline organ dysfunction (%) | |
| Cardiac | 17 (41) |
| Hepatic | 6 (15) |
| Renal | 32 (76) |
| Diabetes | 17 (41) |
Table 1 Baseline characteristics of PMX-treated patients.
Table 2 shows the causes of sepsis or bacteremia. The most common cause of bacteremia was gastrointestinal perforation, which was observed in 11 patients (26.2%). The second was infection from insufficient sutures and pneumonia, which was observed in 5 patients (11.9%). In our center, PMX therapy was performed in patients with various causes of sepsis.
| No. (%) | |
|---|---|
| Gastrointestinal perforation | 11 (26.2) |
| Insufficient suture | 5 (11.9) |
| Pneumonia | 5 (11.9) |
| Liver abscess | 4 (9.5) |
| Cholangitis | 3 (7.1) |
| Pyelonephritis | 2 (4.8) |
| Ileus | 1 (2.4) |
| Suppurative arthritis | 1 (2.4) |
| Phlegmon | 1 (2.4) |
| Cyst of kidney | 1 (2.4) |
| Phlebitis | 1 (2.4) |
| Unknown | 6 (14.3) |
Table 2 Causes of sepsis or bacteremia.
Next we compared clinical effects of PMX therapy (Table 3). PMX therapy significantly increased the average systolic BP from 106.0 mmHg to 115.2 mmHg (p = 0.03). The inotropic score significantly decreased from 14.3 to 8.4 (p<0.01) and the partial SOFA score also decreased from 2.8 to 2.1 (p<0.01). Although the percentage of dobutamine use increased from 7% to 27%, the percentage of norepinephrine/epinephrine and dopamine use decreased from 71% to 46% and from 71% to 66%, respectively. Vasopressors were stopped in four patients at 72 h after the treatment. This suggests that PMX therapy had a beneficial effect in reducing vasopressor use without any relation with the bacterial type or cause of sepsis. In our study, there was no significant improvement in the conventional SOFA score (p = 0.76), PaO2/FiO2 ratio (p = 0.18), and circulating markers of systemic inflammation (p = 0.97 for WBC and p = 0.36 for CRP).
| Before the treatment | 72 h after the treatment | p | |
|---|---|---|---|
| Blood pressure (mmHg) | 106.2 ± 21.2 | 115.2±28.1 | 0.03 |
| Inotropic score | 14.3±10.7 | 8.4±10.2 | <0.01 |
| pSOFA score | 2.8±1.3 | 2.1±1.5 | <0.01 |
| SOFA score | 11.4±3.4 | 11.6±4.6 | 0.76 |
| PaO2/FiO2 (mmHg) | 248.7 ±101.7 | 275.4±113.6 | 0.18 |
| WBC (x 103/mL) | 12.6±11.1 | 12.5±6.8 | 0.97 |
| CRP (mg/dL) | 14.9±10.0 | 16.9±9.9 | 0.36 |
Table 3 Hemodynamic status before and at 72 h after PMX.
Further, we compared decreasing doses of vasopressors between patients with gram-negative bacteria (the GN group) and nongram- negative bacteria (the non-GN group). The GN group consisted of 13 patients, whereas the non-GN group consisted of 29 patients. PMX therapy significantly improved the inotropic and pSOFA scores in both groups (Table 4). Next, we calculated these scores before and after PMX therapy and compared them between the two groups. Changes in BP, the inotropic score, and the pSOFA scores showed no significant differences between the GN and non-GN groups (p = 0.26, p = 0.11 and p = 0.3, respectively).
| GN ( n = 12) | nonGN (n = 29) | p | |
|---|---|---|---|
| BP before PMX | 95.5±18.9 | 110.0±21.4 | 0.04 |
| BP after PMX | 112.2±37.2 | 116.6±23.3 | 0.32 |
| DBP | -14.7±38.6 | -6.6±18.1 | 0.26 |
| Inotropic score before PMX | 17.8 ±10.7 | 12.6±10.6 | 0.08 |
| Inotropic score after PMX | 9.0±7.3 | 8.5±11.3 | 0.44 |
| Dinotropic score | 8.7±9.7 | 4.1±8.8 | 0.11 |
| pSOFA score before PMX | 3.1±0.6 | 2.6±1.5 | 0.18 |
| pSOFA score after PMX | 2.3±1.4 | 2.0±1.5 | 0.67 |
| DpSOFA score | 0.8±1.0 | 0.6±1.0 | 0.30 |
Table 4 Comparison between gram-negative bacteremia (GN) and non-gram-negative bacteremia (nonGN) groups.
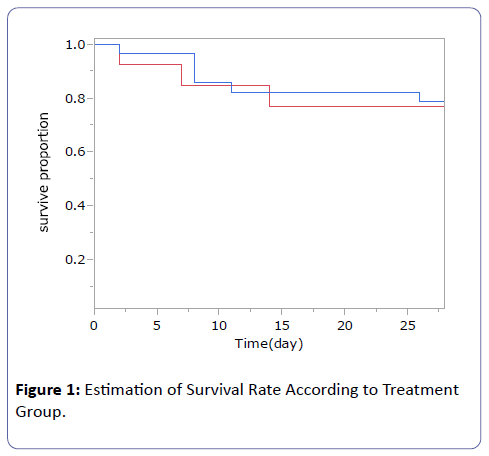
The 28-day mortality also showed no significant differences between the GN and non-GN groups (p = 0.85) (Figure 1). PMX therapy was effective in improving hemodynamic scores in the GN and non-GN groups. This suggests that PMX therapy is useful in improving hemodynamic status in patients with bacteremia caused both by gram-negative and non-gram-negative bacteria.
Discussion
The new findings of the present study are that PMX therapy is useful in improving hemodynamic status in patients with bacteremia caused both by gram-negative and non-gram-negative bacteria, and that lowering vasopressor use also resulted in the improvement of hemodynamic scores, which we employed two different measurements, the inotropic and pSOFA scores. Cruz conducted an RCT in 64 patients and showed that PMX lowered vasopressor requirement, the PaO2/FiO2 ratio, and SOFA and inotropic scores at 72 h after the treatment [7]. The mean BP and SOFA score at baseline was worse in Cruz’s study compared with the present study. This suggested that the population of our study had a relatively better health condition than that of Cruz’s study and that the differences in overall health led to different results; however, both studies consistently showed that PMX has a beneficial effect on these scores. However, different severities of sepsis may cause minor differences in results, such as the improvement in the conventional SOFA scores. Another study also showed favorable effects of PMX therapy on BP, vasopressor use, and cardiac parameters [6]. A systemic review mentioned that PMX improves MAP and decreases vasopressor use [5]. Taken together, it is strongly possible that PMX has beneficial effects on cardiac functions in conjunction with improvement in BP.
The most common bacteria in the present study were E. coli, gramnegative bacteria, but some cultures showed growth of grampositive bacterium. Theoretically, the removal of endotoxins from the circulation is thought to be the primary target of PMX in the treatment of sepsis [2,17]. Further, no significant difference was observed in circulating endotoxin levels after treatment with PMX [18]. This suggests that PMX modulated inflammatory reactions with a decrease in the levels of cytokines such as interleukin-6 and TNF PMX also decreased anandamide and 2-arachidonoylglycerol (2-AG), which are proposed to play a crucial role in the induction of shock-related hypotension [19-24]. Both anandamide and 2-AG are known to increase 4-fold and 3-fold, respectively, in the circulation of patients with septic shock [23]. Endocannabinoids are implicated in the pathogenesis of hypotension associated with septic shock [25]. Removal of these circulating factors by PMX may improve the hemodynamic status of patients with sepsis. Consistent with previous studies, our study showed the effectiveness of PMX therapy against septic shock due to gramnegative or other types of bacteria. The precise mechanisms of how PMX reduces inflammatory activity in sepsis remain unknown. In vitro data showed that the adsorption equilibrium of an endotoxin reached maximum levels at approximately 2 - 3 h [26]. Longer durations of PMX therapy may have a better effect on septic shock compared with the conventional 2-h treatment [27]. This study also supports the hypothesis that the effect of PMX comes not only from the removal of endotoxin but also from the decrease in inflammatory responses. It is very likely that PMX has the potential to absorb not only endotoxins but also other circulating factors related to septic shocks.
The present study has several limitations. First, the sample size was relatively small and the study was performed in a single center. We enrolled all the patients treated with PMX in the study-period and did not calculate sample size suitable for statistical analyses. Most studies on PMX therapy, including RCTs, were performed in 30 - 70 participants [28]. Our sample size was small, but the study results are important because they support the results of several other studies. Another limitation was the retrospective and observational nature of this study.
In conclusion, PMX therapy is effective for improving hemodynamic status of patients with sepsis infected with not only gram-negative but also non-gram-negative bacteria.
Declaration of conflicting interest
None declared.
References
- Shoji S, Minaga M, Sakai Y, Kunimoto T, Takeyama T, et al. (1993) M. Design and development of endotoxin detoxifying column PMX and its clinical application. Jpn J Artif Organ 22: 204-211.
- Tani T, Hanasawa K, Endo Y, Yoshioka T, Kodama M, et al. (1998) Therapeutic apheresis for septic patients with organ dysfunction: hemoperfusion using a polymyxin B immobilized column. Artif Organs 22: 1038-1044.
- Nakamura T, Ebihara I, Shoji H, Ushiyama C, Suzuki S, et al (1999) Treatment with polymyxin by immobilized fiber reduces platelet activation in septic shock patients: decrease in plasma levels of soluble P-selectine, platelet factor 4 and thromboglobulin. Inflamm Res 48: 171-175.
- Nakamura T, Kawagoe Y, Suzuki T, Shoji H, Ueda Y, et al. (2007) Polymyxin B-immobilized fiber hemoperfusion with the PMX-05R column in elderly patients suffering from septic shock. Am J Med Sci 334: 244-247.
- Cruz DN, Perazella MA, Bellomo R, de Cal M, Polanco N, et al. (2007) Effectiveness of polymyxin B-immobilized fiber column in sepsis: a systematic review. Crit Care 11: R47.
- Vincent JL, Laterre PF, Cohen J, Burchardi H, Bruining H, et al. (2005) A pilot-controlled study of a polymyxin B-immobilized hemoperfusion cartridge in patients with severe sepsis secondary to intra-abdominal infection. Shock 23: 400-405.
- Cruz DN, Antonelli M, Fumagalli R, Foltran F, Brienza N, et al. (2009) Early use of polymyxin B hemoperfusion in abdominal septic shock: the EUPHAS randomized controlled trial. JAMA 301: 2445-2452.
- Sato K, Maekawa H, Sakurada M, Orita H, Komatsu Y (2011) Direct hemoperfusion with polymyxin B immobilized fiber for abdominal sepsis in Europe. Surg Today 41: 754-760.
- Mitaka C, Tomita M (2011) Polymyxin B-immobilized fiber column hemoperfusion therapy for septic shock. Shock 36: 332-338.
- Levy MM, Fink MP, Marshall JC, Abraham E, Angus D (2003) SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31: 1250-1256.
- Shore S, Nelson DP, Pearl JM, Manning PB, Wong H (2001) Usefulness of corticosteroid therapy in decreasing epinephrine requirements in critically ill infants with congenital heart Disease. Am J Cardiol 88: 591-594.
- Wernovsky G, Wypij D, Jonas RA, Mayer JE Jr, Hanley FL, et al. (1995) Postoperative course and hemodynamic profile after the arterial switch operation in neonates and infants. A comparison of low-flow cardiopulmonary bypass and circulatory arrest. Circulation 92: 2226-2235.
- Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, et al. (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22: 707-710.
- Moreno R, Vincent JL, Matos R, Mendonca A et al(1999) The use of maximum SOFA score to quantify organ dysfunction/failure inintensive care. Results of a prospective, multicentre study. Intensive Care Med 25:686-696
- Monti G, Terzi V, Calini A, Di Marco F, Cruz D, et al. (2015) Rescue therapy with polymyxin B hemoperfusion in high-dose vasopressor therapy refractory septic shock. Minerva Anestesiol 81: 516-525.
- Sugiura M, Mitaka C et al (2015) Polymyxin B-immobilized fiber column hemoperfusion mainly helps to constrict peripheral blood vessels in treatment for septic shock. Journal of Intensive Care 3:14
- Tani T, Hanasawa K, Kodama M, Imaizumi H, Yonekawa M, et al. (2001) Correlation between plasma endotoxin, plasma cytokines, and plasminogen activator inhibitor-1 activities in septic patients. World J Surg 25: 660-668.
- Amaral AC (2009) Polymixin B hemoperfusion and mortality in abdominal septic shock. JAMA 302: 1968-1970.
- Kushi H, Miki T, Nakahara J, Okamoto K, Kawahara Y, et al. (2006) Hemoperfusion with an immobilized polymyxin B fiber column reduces circulating interleukin-8 concentrations. TherApher Dial 10: 425-429.
- Shimizu T, Hanasawa K, Sato K, Umeki M, Koga N et al (2009) PMX Treatment Study Group: Direct hemoperfusion with polymyxin B immobilized fiber columns improves septic hypotension and reduces inflammatory mediators in septic patients with colorectal perforation. Langenbecks Arch Surg 394: 303-311.
- Wang Y, Liu Y, Sarker KP, Nakashima M, Serizawa T, et al. (2000) Polymyxin B binds to anandamide and inhibits its cytotoxic effect. FEBS Lett 470: 151-155.
- Kohro S, Imaizumi H, Yamakage M, Masuda Y, Namiki A, et al. (2006) Anandamide absorption by direct hemoperfusion with polymixin B-immobilized fiber improves the prognosis and organ failure assessment score in patients with sepsis. J Anesth 20: 11-16.
- Wang Y, Liu Y, Ito Y, Hashiguchi T, Kitajima I et al (2001) Simultaneous measurement of anandamide and 2-arachinoylglycerol by polymyxin B-selective adsorption and subsequent high-performance liquid chromatography analysis: increase in endogenous cannabinoids in the sera of patients with endotoxic shock. Anal Biochem 294: 73-82.
- Ikeda T, Ikeda K, Nagura M, Taniuchi H, Matsushita M, et al. (2004) Clinical evaluation of PMX-DHP for hypercytokinemia caused by septic multiple organ failure. TherApher Dial 8: 293-298.
- Malinowska B, Lupinski S, Godlewski G, Baranowska U, Schlicker E (2008) Role of endocannabinoids in cardiovascular shock. J PhysiolPharmacol 59 Suppl 8: 91-107.
- Shoji H (2003) Extracorporeal endotoxin removal for the treatment of sepsis: endotoxin adsorption cartridge (Toraymyxin). TherApher Dial 7: 108-114.
- Mitaka C, Tsuchida N, Kawada K, Nakajima Y, Imai T et al (2009) A longer duration of Polymyxin B-immobilized fiber column hemoperfusion improves pulmonary oxygenation in patients with septic shock. Shock 32: 478-483.
- Cruz DN (2014) New trends in polymyxin B hemoperfusion: from 2006 to 2013. Blood Purif 37 Suppl 1: 9-13.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences